INTRODUCTION
Myopia is one of the most commonly diagnosed refractive errors in children [1]. The current prevalence of myopia in Europe in the group of patients aged 25-29 ranges between 45 and 50%, and has significantly increased over the past decades [2]. According to estimates, by 2050, half of the global population will be myopic [3]. The etiology of myopia has not been fully explored. The pathomechanism of its development involves both genetic and environmental factors such as eye strain from excessive near work or limited outdoor activity. It is believed that susceptibility to developing myopia and its progression dynamics may be hereditary, while environmental factors are recognized as trigger factors [4]. There is strong evidence confirming that the earlier in life myopia occurs, the higher the degree it reaches in the future [5]. High myopia may cause serious complications, including retinal detachment, glaucoma or cataract, which may lead to blindness [6]. According to the current approach, there is no threshold value for myopia which may be specified as a marking point for complications, as these may occur even with low myopia [7]. Notably, myopia may be of sudden or slow onset. Its progression dynamics is variable, as is the age when stabilization is seen [8]. Regular monitoring of ocular axial length and refractive error should serve as the basis in examination of children with myopia. Preventing the development and halting the progression of myopia involve lifestyle interventions such as increased physical activity outdoors, pharmacological measures, e.g. low concentration atropine eye drops, and optical methods: optical lenses with defocus incorporated multiple segments (DIMS) technology, MiSight soft contact lenses, and orthokeratology [9].
MATERIAL AND METHODS
This aim of this study was to analyze the dynamics of ocular length growth and refraction increase in children and adolescents with myopia. The intended assessment involved the association between the ocular length growth and the patients’ age, the degree of refractive error, and sex, as well as the correlation between an increase in refractive error and patient’s age, the degree of refractive error, and sex.
This retrospective study enrolled 810 patients (1,620 eyes), aged 7 to 17, diagnosed with myopia. Subjects were excluded if they had any of the following criteria: other ophthalmological or advanced systemic disorders, use of methods to slow the progression of myopia during and one year prior to study enrollment. Females represented 63% of the study group, while males represented 37%. They were patients of the Department of Pediatric Ophthalmology with Strabismus of the Medical University Children’s Clinical Hospital in Białystok.
Each patient had their age, refractive error and ocular axial length determined at diagnosis and at follow-ups performed every six months. Patient follow-up periods ranged from 1.5 to 2.5 years, with an average of 2 years. The measurement of ocular length (mean of 5 measurements) was performed in A-scan ultrasonography using a Humphrey device. Refraction (mean of 3 measurements) was determined using an autorefractometer by Topcon, after instilling tropicamide 1% eye drops into the conjunctival sac three times. The patients were divided into three age groups, comprising group 1: patients 7-9 years old, group 2: patients 10-12 years old, and group 3: patients 13-17 years old. Regarding the degree of refractive error, the patients were assigned to another set of groups, comprising group A: patients with low error (up to –4 diopters (D), group B: those with moderate error (from –4 D to –6 D), and group C: those with high refractive error (above –6 D).
Statistical analysis
The statistical analysis was conducted using Statistica 13 PL software. Distribution of variables was tested using the Shapiro-Wilk normality test, and homogeneity of their variance was determined by Levene’s test. The Mann-Whitney U test was used for comparison of non-parametric variables. The differences between the means were assessed using the Kruskal-Wallis test, and also using tests of multiple comparisons. The threshold of statistical significance was set at 0.05 (p ≤ 0.05).
RESULTS
Assessment of mean ocular length growth
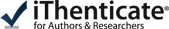
Mean ocular length growth data in particular years of life are presented in Figure 1. As shown in the diagram, after the age of 15 the ocular length growth is smaller than before this age.
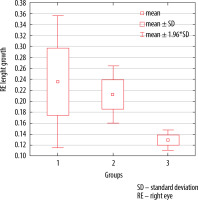
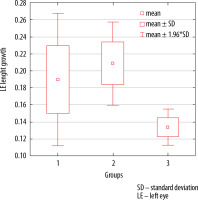
Figures 2, and 3 show statistical data for three age groups.
We found a statistically significant difference in mean ocular length increase for the division by age (for the right eye p= 0.0000, for the left eye p= 0.001). A post-hoc analysis showed significant differences only between group 2 and 3 for both eyes. The group of children aged 10-13 was characterized by greater mean ocular lengths than the group of older children.
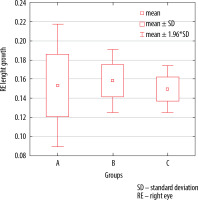
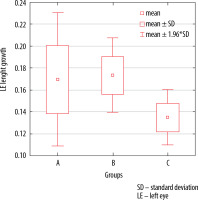
Figures 4, and 5 present statistical data regarding distribution by the degree of refractive error.
No statistically significant differences were demonstrated for mean right and left eye length growth with reference to the division of the study group by the degree of the refractive error, with p= 0.407 for the right eye, and p= 0.943 for the left eye.
Assessment of mean refraction increases
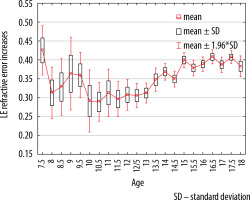
Mean refraction increases are shown in Figure 6. The greatest rate of myopia increase was noted in the group of patients aged 10-12.
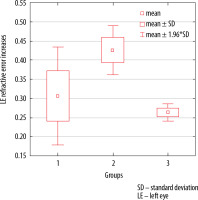
Figures 7, and 8 present the results for particular age groups.
The analysis demonstrated statistically significant differences in mean refractive increases in the right and left eye in particular age groups, with p = 0.000 for the right eye and p = 0.001 for the left eye). A post-hoc analysis demonstrated statistically significant differences only between groups 2 and 3. In the group of children aged 10-12 the mean refraction increase was greater than in the group of older children.
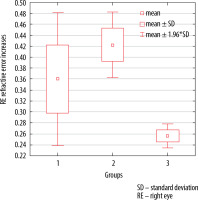
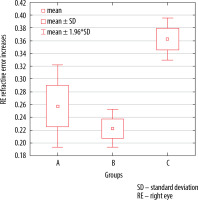
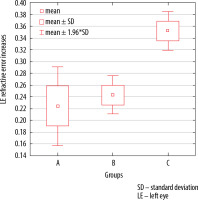
Figures 9-10 present statistical data considering the division according to refraction increases.
A statistically significant difference in mean refraction increase was observed for both the right eye, with p = 0.0000, and the left eye, with p = 0.001. In a post-hoc analysis of the right eye data, group C demonstrated a significantly greater mean myopia increase compared to group B. For the left eye, significant differences were found between all the groups. The group with the highest refractive error showed the greatest mean refraction increase in comparison to other groups.
We noted that each increase in ocular axial length by 1 mm results in an increase in refractive error by mean 2.65 D in the right eye and 2.47 D in the left eye.
Distribution by sex
Our study found that the mean ocular axial length growth was significantly higher in boys than in girls. The difference for the right eye was 0.65 mm (p = 0.0000), and for the left eye 1.03 mm (p = 0.0000).
Mean increase in refractive error for both eyes in the male group (p = 0.665) did not differ significantly from the mean value in the female group (p = 0.278).
DISCUSSION
Myopia has gained the status of an epidemic in developed countries. A rapid rise in the prevalence of this refractive error in children not only entails individual health consequences for a growing group of children, but also makes myopia an important public health issue. Owing to the fact that its etiopathogenesis has not been fully elucidated, myopia continues to be the subject of numerous studies.
There is a general expert consensus that ocular axial length is the best parameter for monitoring myopia and the risk of its development in children [10-12].
Myopia progression has been observed to be the fastest in young children, aged 7-12, and slower in adolescence and adulthood [13]. According to research conducted by the COMET Group, the mean age for myopia to stabilize is 15, while at the age of 24 stabilization occurs in 95% of affected individuals. The age of reaching stabilization and the degree of refractive error are at that point determined by ethnicity [14]. Our study shows that the myopic eyeball is characterized by quick growth from early years of life (Figure 1), and a sudden increase in refractive error (Figure 6) occurs only after 10 years of age. From age 10, axial elongation and refractive error progression display a greater correlation.
Another finding in our study was that ocular length growth by 1 mm is associated with an increase in myopia by 2.47-2.65 D. Prost et al. [15] examined emmetropic children aged 0 to 14 in order to define parameters of a normally developing eyeball. Mean axial emmetropic ocular length in the group of patients aged 7-9 was by 2.99 mm smaller than the mean ocular length in our myopic patients representing the same age group. The difference for the patients aged 10-12 was 2.81 mm. Based on data by Prost et al., one may conclude that emmetropic ocular length growth by 1 mm results in a shift of the refractive error towards myopia (myopic shift) by 1 D. Cruickshank et al. [16] in their study observed that, in the age group of 6-7, ocular length growth by 1 mm caused myopic shift by 3.85 D, compared to 3.1 D in the age group of 12-13.
In 2018 Li et al. [17] published a paper presenting an algorithm predicting progression of high degree myopia. It was a retrospective study based on the analysis of electronic records of a large patient cohort covering a period of 10 years. The algorithm created by these researchers was based solely on progression of myopia measured in diopters. However, it is generally accepted that, in order to create a reliable model of myopia progression, more variables, such as ocular axial length growth or occurrence of myopia in parents are needed as well as environmental data.
In our study, we observed that initially ocular length growth, despite its fast dynamics, is not reflected in a linear increase in myopia. Up to 10 years of age, the value of refractive error is low, growing between 10 to 13 years of age, only to stabilize over the coming years. A rapid increase in myopia after the age of 10 is associated with the ‘growth spurt’ and failure of the optic centers of the eye to compensate for that. Hou et al. [18] detected a correlation between myopia progression and ocular length growth. They also found, as we did in our study, that the greatest ocular length growth occurs up to 13 years of age, which is followed by slowing growth, to reach stabilization. The authors are convinced that ocular axial length growth is the main component in the process of myopia progression.
Our study focused on refractive error and ocular axial length. These parameters together with environmental factors such as outdoor activity or close work will in the future help to develop a model for myopia progression. This may be of help in recognizing the moment when appropriate therapies targeted at inhibiting myopia progression should be instituted.
CONCLUSIONS
The fastest progression of myopia is seen in children aged 10-12. Therefore, these patients should be monitored more often than other age groups. It is also in this group that the possibility of using measures inhibiting myopia progression should be particularly held in mind. Additionally, faster myopia progression is also seen in patients with the initial refractive error > –6 D. Hopefully, the data collected in our study will in the future be used to develop a model of myopia progression.

 ENGLISH
ENGLISH