INTRODUCTION
The cornea is essential for maintaining clear vision and protecting the inner ocular structures. It is susceptible to injuries that may lead to infection and cause impaired vision or blindness. The second most common cause of ocular trauma are foreign body injuries. If an injury is superficial and quickly treated, it does not cause long-term vision defects. Penetrating injuries that reach the endothelium of the cornea may lead to corneal perforation, which may result in serious infection, hyphema, or corneal scarring. Providing immediate and comprehensive help in the emergency department is the key to preserving the optimal corneal function [1].
Thorough medical history and a detailed eye examination, ideally including fluorescein dye, are necessary to correctly determine the type of injury. Initial treatment should involve management of pain and prevention of further trauma. Depending on the type of injury, treatment may require the usage of topical antibiotics, taking swabs from the wound, the removal of a foreign body, and the closure of the laceration or perforation. If the injury is severe, the patient may eventually require corneal transplantation [2].
Acremonium sp. is a genus of fungi typically recognized as an opportunistic pathogen. It usually infects patients who are immunocompromised. The most common fungi responsible for infections are Aspergillus sp., Fusarium, and Candida. It is possible to determine the pathogen responsible for the infection by taking a conjunctival swab [3].
CASE REPORT
A 62-year-old man suffered a corneal injury in his left eye caused by a pumpkin root. The patient presented with severe, constant pain, redness of the eyeball, and blurred vision. The topical antibiotic doxycycline was administered and the patient was sent home.
During the follow-up visit, slit-lamp examination of the anterior segment of the irritated left eye showed a minor corneal ulcer and aqueous-mucous secretion in the conjunctival sac. The patient received topical treatment with eye drops containing a solution of 5 mg/ml of levofloxacin and 1 mg/ml of dexamethasone, 0.2% fluconazole, and 50 mg/g dexpanthenol.
A subsequent visit showed no clinical improvement and the slit lamp examination showed extensive tissue destruction in the left eye, along with the lack of preserved epithelial continuity of the cornea. Confocal microscopy examination revealed numerous Langerhans cells at the basal layer. It is worth noting that the examination did not show any Acanthamoeba cysts or fungal cells, although the assessment was difficult due to the inflammation of the epithelial tissue.
Throughout the next 5 weeks, the patient returned for multiple follow-up visits and received topical medications including 0.1% dexamethasone, 50 mg/g dexpanthenol, 5 mg/ml moxifloxacin, 1% tropicamide and 0.2% fluconazole, 6 times a day each.
Six weeks later, the patient was admitted to the emergency department, presenting with constant pain in his left eye. Visual acuity was poor, determined as light perception with localization.
The patient received an amniotic graft. The procedure was successful, however ten days later the patient complained of severe pain in the left eye. The patient received antibiotics and steroids and an artificial protective lens.
A month later, the patient was admitted for urgent care to the clinical hospital due to constant pain in the left eye (Figure 1). The slit-lamp examination revealed inflammatory exudate in the anterior chamber, and central opaqueness of cornea. Visual acuity assessment indicated light perception without localization. Therapeutic keratoplasty was performed. The amniotic membrane graft was removed and the donor cornea was affixed.
The fluid of the anterior chamber was tested for the presence of bacterial and fungal organisms, resulting in the growth of Acremonium sp. Following the results, voriconazole treatment was administered, followed by dexamethasone, moxifloxacin, and azathioprine. The patient’s condition gradually improved, as he was admitted every 2 weeks for the following doses of antibiotics and steroids.
Recovery after keratoplasty resulted in slight improvement in the patient’s vision. The slit-lamp examination showed less inflammatory exudate in the anterior chamber and the cornea no longer appeared as opaque as before. The patient discontinued his complaints of pain.
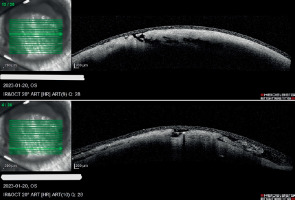
Throughout the whole treatment process, the patient was admitted every 2 weeks for a 2-week hospitalization, where he received medications and his visual acuity was assessed thoroughly (Figure 2). It is important to note that the patient’s vision improved after he had received an amniotic graft, and it deteriorated to light perception with uncertain localization.
Figure 2
Slit-lamp examination shows consecutive stages of healing: A) 27.01; B) 19.02; C) 22.02; D) 1.03; E) 3.03.2023.
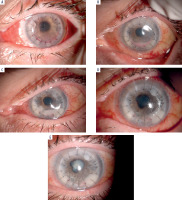
Unfortunately, several weeks later, the patient was again admitted to the Ophthalmology Clinic with severe pain in the same eye (Figure 3). Slit-lamp examination showed massive inflammatory exudate in the shallow anterior chamber, along with redness of the conjunctiva and an opaque cornea with vis- ible necrotic tissue and perforation in the medial part. Visual acuity was assessed as light perception without localization. The conjunctival swab indicated reinfection of Acremonium sp. Due to the patient’s worsening condition, the enucleation of the left eye was performed.
DISCUSSION
We report a case of a patient with corneal fungal infection of Acremonium sp. Despite intensive treatment and graft transplantation the eyeball was eventually enucleated.
Fungal infections continue to pose a significant clinical challenge. During its course, the infection can spread deep into the eye, leading to endophthalmitis or even panophthalmitis [4]. They occur more frequently in patients with corneal injuries, especially of plant origin and those with soil-contaminated injuries, contact lens wearers and individuals chronically using steroids [5, 6].
Diagnostic evaluation is crucial, including a thorough slit-lamp examination. Standard practice should also include obtaining corneal scrapings for cultures with antibiotic susceptibility testing, as well as for direct microscopic examination [4, 7]. It is worth noting that, although they are the gold standard in the diagnosis of fungal keratitis, cultures require a longer period of time than their bacterial counterparts. Molecular methods are also used in diagnosis, which can help determine the exact etiology of the infection [4].
Since the first case of Acremonium sp. eye and surrounding tissue infection in 1971, until 2019 the number of reported cases worldwide remained scarce, totaling only 82 [3, 8]. In 32 of the documented cases there was a history of trauma, 13 with vegetable matter and 4 with wooden sticks [8].
Despite its rarity, Acremonium sp. has become a more common pathogen in ocular infections. This pathogen demonstrated a predilection for patients receiving steroid therapy and those who are immunocompromised. Previous cases have shown varied outcomes and treatment, reflecting the complexity of managing the infection. Treatment included keratoplasty, vitrectomy and the use of antifungal medication, such as amphotericin B, voriconazole, itraconazole and terbinafine. In the cases where treatment details were provided, the results varied, with cases resulting in full recovery, while others lacked such information [3, 8]. There was only one case of Cephalosporium endophthalmitis where enucleation was necessary [8, 9].
Scientific sources suggest natamycin used topically as a first-line treatment, especially in Fusarium spp. infections. If natamycin treatment is ineffective, second-line treatment includes voriconazole or amphotericin B [6].
In most cases antifungal drugs are used topically, however, systemic, intrastromal or intracameral routes may also be used. Treatment of fungal infection still poses difficulties due to the low bioavailability of the drug used in treatment and the lack of clear guidelines for the management of such infections [1, 10].
A particular form of high-risk corneal transplantation, therapeutic corneal transplant, also known as hot grafting, is carried out mainly in patients suffering from infections. The aim of this procedure is to remove necrotic tissue and spare the eye as an organ. Patients who undergo hot transplantation for infectious reasons are at high risk of graft rejection. Treatment to prevent graft rejection should be introduced after the procedure. Despite its higher risk most patients after high-risk corneal transplantation still experience significant improvements in visual acuity. Unfortunately, many cases may still require enucleation [12].
Enucleation is primarily indicated in malignant tumors, it is performed in cases of pain in the blind eye, severe trauma or infection leading to irreversible blindness [13]. In our case, it was the final treatment option due to the lack of other therapeutic possibilities, exacerbated inflammation and corneal ulceration. The goal was to alleviate the patient’s symptoms and prevent the transmission of infection to the other eye. Since the surgery, the patient’s condition has improved and he has not reported any symptoms from the other eye.
CONCLUSIONS
The case presents the story of a patient whose initial simple case of eye trauma with a biological material led to permanent loss of one eye. Initially, the cornea was not swabbed and cultures were not taken, which delayed the implementation of the targeted treatment.
During the following months symptoms fluctuated, alternating between periods of improvement of the patient’s condition and exacerbation of the infection with severe pain, leading to therapeutic keratoplasty. Despite successful surgery and adequate adaptation of the transplanted corneal graft, the patient suffered from recurrent symptoms and was frequently hospitalized.
Ultimately, what initially appeared to be mechanical trauma, usually treated with a short course of antibiotics, resulted in enucleation due to continuous infection, the absence of proper response to pharmacological and surgical treatment, deterioration of the patient’s both physical and mental state, and the insufficiency of other treatment options. It is worth noting that any case of a corneal injury may result in a difficult-to-control infection and should be treated with antibiotics. When it is unmanageable, the implementation of surgical treatment may be optimal for the patient. As enucleation is considered as the last-line treatment, it may eventually be found to be helpful, after other options are exhausted.

 ENGLISH
ENGLISH