INTRODUCTION
With life expectancy steadily increasing, age-related diseases such as cataracts and presbyopia continue to pose health challenges that cause significant visual impairment in both low- and high-income countries [1]. Multifocal lenses have been a solution for these patients to at least partially restore the ability to see from different distances. Unfortunately, they are not free of side effects such as glare, halo or starbursts, especially while looking at car headlights and street lamps when driving at night [2-6]. Extended depth of focus (EDoF) lenses are intended to answer the needs of middle-aged and elderly patients who still want to be professionally active. There are currently many of them on the market to choose from, such as Mini Well Ready (SIFI Medtech, Catania, Italy), TECNIS Eyhance ICB00 (Johnson and Johnson Vision, Jacksonville, FL), Tecnis Symfony ZXR00 (Johnson and Johnson Vision, Jacksonville, FL), AcrySof IQ Vivity (Alcon Inc., USA), and LuxSmart IOL (Bausch & Lomb GmbH, Berlin, Germany). One of them is the AT LARA 829MP (Carl Zeiss Meditec, Jena, Germany) lens, but there are not many studies available with the results of long-term follow-up after its implantation [7, 8].
Here it should be noted that nowadays, a large percentage of people over 60 years of age drive cars, and in this group of patients we can expect cataracts to be a significant cause of vision impairment. Therefore, it is important to know how they behave on the road as drivers and whether the implantation of the AT LARA 829MP intraocular lenses (IOLs) is safe for people driving motor vehicles. Additionally, we should also pay attention to mobility. A significant percentage of older patients are longer active not only professionally, but also physically, and the decline of visual and motor skills may significantly impede everyday functioning and increase the risk of falls. Currently, there are sparse data on visual-mobility performance in patients with pseudophakia, and objective tests are available to examine it.
The purpose of this article is to present our 12-month observations after binocular implantation of AT LARA 829MP IOL and compare them with the results available in the literature. An additional value of this work is to show the results of tests for professional drivers and the results of hand-eye coordination tests.
MATERIAL AND METHODS
The prospective study included patients after uncomplicated bilateral cataract surgery with implantation of AT LARA 829MP at the 2nd Department of Ophthalmology in Szczecin, Poland. All patients wanted to become spectacle independent or were willing to accept minimal spectacle correction for prolonged reading, and they were informed about the advantages and disadvantages of EDoF IOL implantation. The study complied with the Declaration of Helsinki and was approved by the local ethics committee. Written informed consent was obtained from all patients.
The inclusion criteria for the EDoF IOL implantation included: age of 40-70 years, bilateral cataract or refractive surgery, pupil size of 3-6 mm in dim light, preoperative corneal astigmatism below 0.75 D, hyperopic presbyopia, the patient’s motivation for spectacle independence or the patient being willing to use limited spectacle correction for prolonged reading, no diseases other than cataracts, and the willingness and ability to comply with scheduled visits.
The exclusion criteria included: ocular diseases other than cataract such as macular disease, eye movement disorders, amblyopia, dry eye syndrome, diseases of the cornea and previous corneal refractive surgery, pupil abnormalities, glaucoma, pseudoexfoliation syndrome, high myopia with axial length (AL) ≥ 25.5 mm and hyperopia (AL ≤ 21.5 mm), lifestyle and work-related factors, such as unrealistic visual expectations, patients demanding visual precision, i.e. pilots, professional drivers, architects, etc., patients satisfied with reading glasses, individuals over 70 years of age due to likely difficulties associated with problems in neuroadaptation to new optical conditions as well as personality-related factors, such as mental disorder of any type, patients dissatisfied with progressive spectacle lenses, history of stroke and dyslexia, and IOL power out of range.
Intraocular lens
The main characteristics of the AT LARA 829MP are presented in Table I.
Table I
Specifications of AT LARA 829MP EDoF IOL
Preoperative and postoperative examination
Preoperatively, all patients underwent a complete ophthalmic examination, including uncorrected visual acuity, objective refraction, corneal topography (CASIA2, TOMEY), slit lamp biomicroscopy of the anterior and posterior segments with Volk lens, Pascal tonometry and biometry (IOL Master 700, Carl Zeiss Meditec AG).
The clinical evaluation performed on all subjects 12 months after surgery included the following: autorefraction; binocularly: UDVA (logMAR ETDRS chart at 4 m), UNVA (at 40 cm) and UIVA (at 60, 70, 80 cm); defocus curve with ETDRS chart positioned at 6 m assessed under photopic conditions – the change of VA by addition of 0.5 D increments at each step towards hyperopia (0 to +1.5 D) and myopia (0 to −3.0 D); distance contrast sensitivity (CS) (2.5 m) assessed under photopic (85 cd/m2) and mesopic (3 cd/m2) conditions, near CS (40 cm) assessed under photopic conditions (1.5, 3, 6, 12, and 18 cycles/degree, CSV-1000, Functional Acuity Contrast Test – FACT); spectacle independence; subjective perception of photic phenomena (glare and halo); patient satisfaction (modified VFQ-25) [9]; and postoperative complications.
In order to compare CS, we created a control group in the same age range (there were no statistically significant differences between the groups) and without ocular diseases, which we also examined using the CSV-1000 test and FACT.
Sixteen patients underwent qualifying tests for drivers.
The study was conducted at the West Pomeranian Occupational Medicine Center. The patients underwent tests required to obtain a positive decision for a professional driver, which in Poland are covered by the Road Transport Act of September 6, 2001 and the Regulation of the Minister of Health of August 29, 2019 on medical examinations of persons applying for driving licenses and drivers [11]. These tests include (with the exception of VA and visual field tests, which are required for every driving license): color recognition (Ishihara test), assessment of binocular vision (cover test, TNT test), scotopic vision (BDT test), CS, and glare sensitivity (Optovist vision test).
Surgical technique
Phacoemulsification (Stellaris, Bausch & Lomb) was performed in both groups by the same surgeon (WL) under topical (Alcaine) and intraocular (1% lidocaine) anesthesia. The IOL was implanted through an average1.8-mm clear corneal incision. The size of the capsulorhexis was approximately 5 mm. After cataract removal and cortical aspiration, the fully preloaded IOL (AT LARA 829MP IOL with BLUEMIXS 180 injector/cartridge set; Carl Zeiss Meditec) was implanted into the capsular bag in all cases. The IOL power was calculated using optical biometry (IOL Master, Carl Zeiss Meditec, Jena, Germany) and the SRK-T (for axial length from 22 to 24.5 mm) or Hoffer Q (axial length below 22 mm) formulas. The target refraction was a slight myopia (–0.5 D). Surgery of the second eye was performed one month after the first.
Postoperatively, all patients used an antibiotic, a steroid, a non-steroidal anti-inflammatory, and moisturizing drops for 4 weeks.
Motility coordination
Nineteen patients underwent motility coordination tests.
Mobility evaluation: The Timed Up and Go (TUG) test was used to assess mobility. In the TUG test, the time that a participant needed to rise from a chair, walk 3 m, turn around, walk back and sit down on the chair was recorded [10]. During the test, the participants wore regular comfortable footwear and did not use any mobility aids (e.g. a cane). The test was performed twice, and only the better result was analyzed in this study. The normative values for the TUG test were as follows: 10 seconds or less indicated normal mobility, 11-20 s were considered to be within the normal limits for frail older patients, and above 20 s indicated functional disability.
Postural stability evaluation: The bilateral dynamic postural stability test was carried out using the Biodex Balance System SD (Biodex Medical Systems Inc, Shirley, New York, USA). The examination started by having the patient stand on a static balance platform in order to obtain a correct center of mass, which was displayed on a monitor and subsequently provided real-time information about the posture. The test was performed without shoes, and foot position was recorded using coordinates on the platform’s grid to ensure the same stance and, therefore, consistency across subsequent test trials. In the postural stability test, the participants were instructed to balance themselves with a fixation point kept at the center of a target on the screen. The dynamic postural stability test was performed using the standard software protocol, i.e. three trials of 20 s each at a stability level of 8-12, with 10 s of rest between the test trials. The average value of three trials was considered for further analyses (overall stability index, in degrees).
Statistical analysis
Descriptive statistics were presented as means, standard deviations (SD), and minimum and maximum values. The assumption of normal distribution was checked using the Shapiro-Wilk W test. Comparison of the data between two groups was performed with the Mann-Whitney U test with corrections for small samples. Calculations were provided using Statistica software. Results were considered as statistically significant at p < 0.05.
Bioethical standards
All procedures performed in the study involving human participants were in accordance with the ethical standards of the Pomeranian Medical University Ethics Committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Informed consent was obtained from all enrolled study participants.
RESULTS
The study included 40 eyes of 20 patients (6 men, 14 women) with a mean age of 63.8 ±6.8 years (ranging from 40 to 70). All patients underwent binocular uncomplicated phacoemulsification with implantation of AT LARA 829MP.
At the 1-year follow-up, the mean cylinder, and SE values were –0.55 ±0.29 D, and –0.67 ±0.29 D, respectively (Table II). Approximately 42% of the eyes (17/40 = 42.5%) were within ±0.50 D and 95% (38 of 40) were within ±1.00 D of SE correction. 70% of the eyes (28 of 40) were within ±0.50 D and 97.5% (39 of 40) were within ±1.00 D of cylinder correction.
Table II
Postoperative visual and refractive outcomes
Visual outcomes
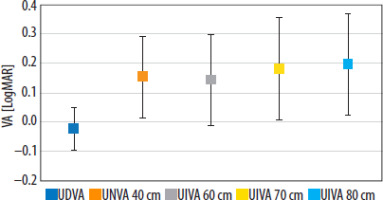
Figure 1 shows the postoperative mean binocular VA at different distances. Twelve months after the surgery, 80% of patients (16 of 20) achieved UDVA 20/20 or better. The mean UDVA was –0.03 ±0.07 logMAR, while all eyes (40 of 40) and patients (20 of 20) had a minimum UDVA 0.12 logMAR.
The percentage of patients who achieved binocular UIVA of 20/40 or better was 95% (19 of 20) at 60 cm, 75% (15 of 20) at 70 cm and 75% (15 of 20) at 80 cm. The mean UIVA was 0.14 ±0.16 logMAR at 60 cm, 0.18 ±0.17 logMAR at 70 cm and 0.2 ±0.17 logMAR at 80 cm binocularly.
Of all patients, 90.0% of patients (18 of 20) achieved UNVA of 20/40 or better. The mean UNVA was 0.15 ±0.14 logMAR.
Defocus curves
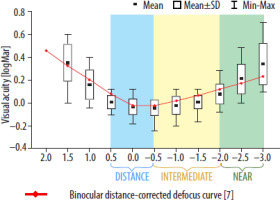
The binocular defocus curve is shown in Figure 2. The binocular defocus curve was plotted using lenses ranging from +1.50 to –3.00 D. The patients with the AT LARA 829MP lens achieved good visual acuity across all distances. Mean visual acuity was greater than 0.1 logMAR and was observed for defocus levels between −2.0 D and +0.50 D. The mean VA at distance (range from +0.5 D to –0.5 D), intermediate (range from –0.5 D to –2.0 D), and near (range from −2.0 D to –3.0 D) was −0.02 ±0.07 logMAR, 0.01 ±0.09 logMAR, and 0.21 ±0.17 logMAR, respectively. The best VA (–0.04 ±0.07) was obtained at –0.50 D vergence, corresponding to the border between the far and intermediate focus.
Our results correspond to the data from the literature, as shown in the Figure 2.
Spectacle independence
At 1 year, all patients (n = 20) achieved spectacle independence for intermediate and distance vision. Six patients reported the need for near glasses – in scotopic conditions all of them, in photopic conditions only 4.
Contrast sensitivity
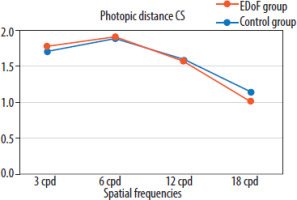
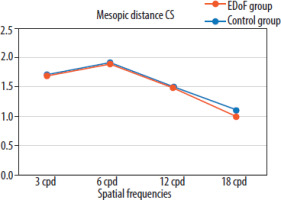
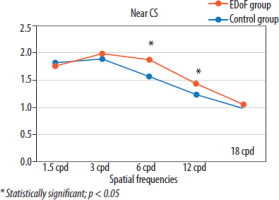
Figures 3 and 4 show the mean binocular CS values under photopic (85 cd/m2) and mesopic (3 cd/m2) conditions for far distance compared to the age-matched control group. Contrast sensitivity was similar under photopic and mesopic conditions. We found no statistically significant differences between patients with EDoF IOLs and the control group (p > 0.05). Figure 5 shows the mean binocular CS values under photopic conditions for near distance. Statistically significant differences in favor of the control group (p < 0.05) occurred for the frequencies of 6 cpd and 12 cpd.
Photic phenomena
Seventy-five percent (15 of 20) and 70% of patients (14 of 20) had complaints of halo and glare, of varying degrees of severity. Table III shows the distribution of postoperative dysphotopsia symptoms. Glare and halo perception was analyzed in terms of frequency and severity. Frequency was rated on a 5-point scale (1 – all the time, 5 – none). Halo level of perception was slightly more pronounced than glare (3.85 ±0.99 vs. 3.95 ±0.83). Severity was rated on a 4-point scale (0 – none, 4 – very intensive). Again, the level of halo perception was slightly more severe than glare (1.3 ±1.22 vs. 1.2 ±1.11).
Patient questionnaire
Table IV shows the responses to individual items on the modified VFQ-25 (scale 1-5; 1 – best, 5 – worst). Good scores were obtained for all aspects, with the worst score associated with night driving (2.19 ±0.98). Overall satisfaction with the quality of vision achieved was high (1.9 ±0.55).
Table IV
Modified VFQ-25 scores (scale 1-5;1–best, 5 – worst)
Postoperative complications
No severe postoperative complications were noted over the 1-year follow-up. Three patients developed significant opacification of the posterior capsule and underwent Nd:YAG laser capsulotomy.
Effect of patients’ visual neuroadaptation after binocular implantation of AT LARA IOLs on mobility and postural stability
Descriptive and statistical values for mobility and dynamic postural stability in the patient and control groups are shown in Table V.
Table V
Descriptive and statistical values for mobility, static and dynamic postural stability tasks in the groups of patients and controls
| Mobility/Stability index | Patients (n= 18) Median (IQR) | Control group (n= 19) Median (IQR) | p (effect size) |
|---|---|---|---|
| TUG (s) | 7.330 (1.242) | 7.630 (1.340) | 0.796 (0.053) |
| OSI (degree) | 0.950 (0.525) | 1.100 (0.300) | 0.418 (0.158) |
In the functional tests, patients did not differ significantly from controls in terms of mobility (TUG) (p > 0.05, effect size = 0.053). In both groups, the median value of TUG indicated normal mobility performance (< 10 s). Similarly, in the dynamic postural balance task, there was no statistically significant difference between the groups of patients and controls (p > 0.05, effect size = 0.158).
Professional driver examination
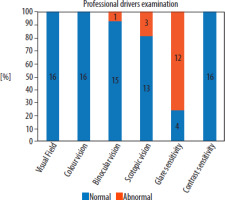
The results of the survey of professional drivers are presented in Figure 6. All 16 examined patients achieved correct test results in terms of visual field, color recognition, and CS. One patient had an abnormal result in the binocular vision test (1 of 16 = 6.25%), 3 in the scotopic test (3 of 16 = 18.75%), and 12 patients presented abnormal results of the glare sensitivity test (12 of 16 = 75%).
DISCUSSION
Our long-term results, after binocular implantation of AT LARA 829MP IOLs, in a selected group of patients, show that these lenses provide very good far and intermediate vision and satisfactory near vision, with a high level of overall satisfaction after the surgery. AT LARA 829MP IOL also provided patients with proper mobility and postural stability in both dynamic and static conditions. However, when we take into account the ophthalmological criteria for professional drivers in Poland, the increased sensitivity to glare that occurred in majority of our patients is an exclusion factor in this professional group.
As we know, binocular VA is better than monocular [12] – this is why we focused on the binocular examination of patients. In our study, we adopted slight myopia (–0.5 D) as the target refraction (which was discussed with patients before the surgery) to achieve better near vision while maintaining very good vision at far and intermediate distances, as shown in the available literature (but with different lenses) [13, 14]. In the literature, there have been only two published articles about binocular implantation of AT LARA 829MP IOLs with a similar 12-month follow-up, and both adopted emmetropia as a target refraction [7, 8]. The consequence of the slight myopic refraction we assumed is that our patients achieved slightly better near visual acuity (0.15 ±0.14 logMAR) compared to the results of Ganesh et al. (0.16 ±0.09 logMAR) or Schallhorn et al. (0.28 ±0.13 logMAR) [7, 8]. In our study, UDVA results were similar or slightly worse than those presented in other long-term studies, but UIVA performed worse compared to other follow-ups with a similar period [7, 8]. This may be related to the slight myopic refraction [13, 14].
Our patients with the AT LARA 829MP lens achieved good visual acuity at all distances on the defocus curve. The mean binocular VA was greater than 0.1 logMAR and was observed for defocus levels between –2.0 D and +0.50 D. Meanwhile, in the article by Reinhard et al., 1 month after the surgery, in this defocus range the mean VA is higher than 0.1 logMAR [15]. In our study, the mean VA for distance, intermediate, and near was (in logMAR) −0.02 ±0.07, 0.01 ±0.09, and 0.21 ±0.17, respectively. In the article of Ganesh et al., the mean binocular corrected distance vision was −0.02 logMAR, and the mean intermediate and near VAs were 0.01 and 0.16 logMAR, respectively [7]. The results are very similar, although it is worth noting that our patients were examined without correction.
In this study, binocular CS for distance was almost equal under photopic and mesopic conditions. We found no statistically significant differences at far distance between patients with AT LARA 829MP IOLs and the age-matched control group (p > 0.05). For near distance, statistically significant differences in favor of the control group (p < 0.05) occurred only for the frequencies of 6 cpd and 12 cpd. Therefore, it can be generally stated that after implantation of these EDoF lenses, CS is very good for distance in all light conditions and slightly worse for near, but only at high spatial frequencies. Analyzing the results presented by other authors, the mean values of CS in photopic conditions in our patients were slightly higher for all spatial frequencies than in the studies of Ganesh et al. [7] and Reinhard et al. [15]. To the best of our knowledge, this is the only study comparing binocular CS in patients with the AT LARA 829MP lens with a control group with natural lenses. Therefore, it is reasonable to conclude that the technology used in the AT LARA 829MP lens does not significantly affect CS.
Despite the expectations that the EDoF lens should be free from glare and halo [16, 17], in our case these were frequent, but with a low degree of perception. The assumption was that these lenses provide very good visual acuity with a significant reduction in the occurrence of photopic phenomena that are commonly associated with multifocal lenses [18, 19]. However, based on the comparative analyses of both groups available in the literature, there are no significant differences in the occurrence of these phenomena [20-25]. In multifocal IOLs, one image is in focus, while the out-of-focus image is neuronally suppressed (simultaneous vision) yet still produces such unwanted dysphotopsia [26]. All diffractive IOLs are known to cause halos to some extent (the disadvantage of diffractive designs is the perception of photic phenomena – arising from the superposition of multiple images on the retina) [27, 28]. In our patient group, the incidences of glare and halo were high (70% and 75%, respectively), and these effects occurred despite the fact that more than 12 months of neuroadaptation had passed after the surgery. A high percentage of dysphotopsia was also reported in other studies, with up to 60% of patients reporting difficulties with the perception of visual phenomena after surgery [7, 29, 30]. Thus, as we noted, the EDoF technology presented in AT LARA IOL does not protect patients’ eyes against unwanted effects.
In the present study, we also evaluated patients’ experiences with everyday aspects such as reading newspapers, using computers or night driving to understand patients’ satisfaction in their daily lives. Based on the results of the modified VFQ-25 questionnaire, it can be concluded that the most prominent difficulty for patients is driving in scotopic conditions, which in our opinion is associated with the occurrence of glare and halo in these patients. In other studies, up to 55% of patients also reported a problem with driving at night [7, 15].
Another criterion that is particularly important for patients is achieving independence from glasses after the surgery. All our patients achieved spectacle independence for intermediate and distance vision, and 70%, as a consequence of slight myopic refraction, became completely independent of near vision glasses, compared to 39.2% for Reinhard et al. [15] and 87% for Ganesh et al. [7]. However, in all studies the overall satisfaction with visual acuity and quality of life after the surgery is rated highly by patients [7, 15]. Nevertheless, it is difficult to compare patient satisfaction scores due to the use of different scales.
The Reinhard et al. study demonstrated good vision after implantation of AT LARA 829MP and TECNIS Symfony EDOF IOLs. Vision at all distances, photic phenomena, spectacle independence, and patient satisfaction were comparable between these lenses. Looking at the single-sided depth of field, monocular depth of focus was significantly better for the eyes with AT LARA 829MP compared to the eyes with TECNIS Symfony, with no significant difference for binocular depth of focus [15]. In Guarro et al.’s article, which compared three EDoF lenses (the non-diffractive IOL AcrySof IQ Vivity and two diffractive IOLs – AT LARA 829MP and TECNIS Symfony ZXR00), the diffractive EDoF models produced similar visual disturbances, which were worse than those produced by the Vivity IOL [31]. According to Baur, under laboratory conditions, the non-diffractive AcrySof IQ Vivity appears to have a smoother transition from far to intermediate range than Symfony ZXR00 and AT LARA 829MP, which suggests that this IOL may induce fewer halos than the diffractive IOL models [32].
There is no study comparing the results of patients after binocular implantation of AT LARA 829MP lenses with patients after binocular implantation of trifocal lenses, but we found comparisons of trifocals and another EDoF using diffractive technology – TECNIS Symfony [20-25, 33-36]. If we take into account the most common parameters for evaluating IOLs, i.e., visual acuity at various distances, defocus curve, CS, occurrence of photopic phenomena, independence from glasses, and subjective assessment of patients, no significant differences were detected. The only distinct difference between TECNIS Symfony and trifocal lenses is a much better UNVA in the case of the latter, which is also confirmed by the defocus curve. Therefore, since the lens we tested belongs to the same group as TECNIS Symfony, it can be concluded that there are no marked differences between diffractive-EDoFs (including AT LARA 829MP) and trifocal lenses, apart from near vision.
To the best of our knowledge, this is the first study to examine the effect of visual neuroadaptation after binocular implantation of AT LARA 829MP IOLs on two essential daily tasks – mobility and postural control. Our data show that functional capacity in terms of mobility and dynamic postural stability tasks did not differ significantly between patients after the 12-month period of neuroadaptation and the control group. The processing for controlling postural instability is determined by the integration of three sensory modalities, i.e. visual, vestibular, and somatosensory [37]. It has been reported that, among these three sensory modalities, the visual system is predominantly used to maintain a standing posture, since vision disturbance causes larger postural sway during quiet standing than vestibular and somatosensory disturbances [38]. Moreover, during dynamic movement control, the nervous system automatically adjusts its emphasis on other systems and induces inter-modality reweighting [39]. Taken together, the results of this study indicate that the sensory integration during mobility and dynamic postural control tasks was not affected 12 months after binocular implantation of AT LARA 829MP IOLs. Therefore, it can be assumed that the risk of injuries during normal life activities will not increase.
After analyzing the results of the modified VFQ-25 questionnaire, we noted that patients report difficulties with driving at night and frequent occurrence of photic phenomena. Therefore, we decided to check whether patients after implantation of AT LARA 829MP lenses would successfully pass professional driver tests. Such patients may have a problem with cataracts and visit ophthalmologists to remove the opacification lens and qualify for the implantation of a new one, e.g. a multifocal or EDoF one. Considering that the average age of our patients is 63.8, this group could also include potential professional drivers. Therefore, we did not find sufficient information about how AT LARA IOL behaves in this group of patients. This is why we also examined patients in terms of obtaining a professional driving license in Poland and, to the best of our knowledge, this is the first study describing the ability of patients with EDoF lenses to obtain such a license. Polish law is quite restrictive as far as this group is concerned, and professional driving requires (apart from the appropriate visual acuity and field of vision tests required everywhere) positive results of the following tests: binocular vision, color recognition, scotopic vision, and sensitivity to glare and contrast [40, 41]. Seventy-five percent of our patients had an abnormal glare sensitivity test result and 19% of patients had abnormal scotopic vision, which, according to Polish guidelines, is a contra indication to obtaining a professional driving license. Auffarth et al. analyzed contrast and glare sensitivity in patients with multifocal IOLs (3M 815LE and 825X) and found that 70% of patients after surgery did not meet the minimum driving license requirements according to the German Society of Ophthalmology (DOG) and showed reduced glare sensitivity and contrast values after surgery [42]. Upon examining the ophthalmic criteria for professional drivers in other countries, we noted that many countries do not take into account the scotopic vision and glare sensitivity tests [43-48]. From our point of view, this is not a good idea, as increased sensitivity to glare and incorrect scotopic vision are a possible cause of riskier behavior on the road and a higher frequency of traffic accidents [49-51].
The purpose behind introducing EDoF lenses in clinical practice was to improve intermediate vision with a minimal impact on far vision and with simultaneous acceptable near visual acuity, as well as to eliminate the overlapping of near and far images caused by multifocal lenses, thereby eliminating the halo effect [18]. Analyses of EDoF and multifocal lenses show that these goals have not been fully achieved by the former [20, 23, 24, 33-35]. The new concept of EDoF lenses is monofocal IOLs with enhanced intermediate vision, which do not impair contrast sensitivity and do not cause photic phenomena, while improving intermediate and near vision in comparison to typical monofocal lenses. Study results demonstrate that mono-EDoF IOLs do not show significant differences in UDVA, UIVA [51- 53] and in one study also UNVA [51], with less glare and halo [51] compared to conventional EDoF IOLs; however, this requires further comparative trials. If we compare our binocular VA results with those of mono-EDoF patients, our study group achieved better UDVA and mostly also UNVA and UIVA [53-56] as a result of planned slight myopia, but with a worse incidence of photic phenomena. In the work of Huh et al. [57], the occurrence of photopic phenomena was also much lower than ours. This is in line with the assumptions of mono-EDoF lenses.
CONCLUSIONS
This is the first study describing the quality of life and vision after bilateral implantation of EDoF AT LARA 829MP lenses in such an extensive scope. However, the small group of patients is undoubtedly a weakness of our study. Our results show that AT LARA provides excellent visual function but still with high frequency of dysphotopsia. Further studies in large groups of patients are necessary to demonstrate that mono-EDoF lenses will be comparable in terms of VA to conventional EDoF, but with lower frequency of photic phenomena. Perhaps thanks to this, mono-EDoFs will turn out to be a new method that will not limit the safety of car driving.

 POLSKI
POLSKI