INTRODUCTION
The constant improvement of quality of new intraocular lens models may contribute to the improvement of the patients’ quality of life. In recent years, many new intraocular lens models have been designed, namely: accommodative and pseudo-accommodative lenses, bifocal, trifocal, multifocal and extended depth of field lenses.
Monofocal lenses do not have side effects typical for multi-focal or EDOF lenses but they only provide good vision from one distance (far or near). The implantation of multifocal intraocular lenses brings many potential benefits in certain groups of patients, allowing the patient to focus on distant, intermediate and close objects, however, it may also be associated with side effects such as: reduced contrast sensitivity, worse night (scotopic) vision, as well as presence of unwanted optical phenomena, e.g. glare, halo, or starburst effects. The halo effect is characterized by the perception of luminous rings around light sources (such as street lamps or car headlights), whereas glare and starburst – caused by splitting of the light rays from a point source – occur in low lighting conditions and can be particularly troublesome at night, as they impair driving performance.
These unwanted optic phenomena might negatively influence patients’ quality of life and decrease patients’ satisfaction with cataract surgery.
The aim of this study was to assess the quality of life in patients after bilateral cataract extraction using phacoemulsification, who had an artificial lens (IOL) implanted in both eyes: either an extended depth of focus (EDoF), multifocal (MIOL), bifocal (Bi), or a standard monofocal acrylic foldable intraocular lens.
MATERIAL AND METHODS
The study group consisted of 100 patients (79 women and 21 men) who underwent phacoemulsification with binocular IOL implantation or various lenses: either an extended depth-of-field EDoFTecnis Symfony (n = 20), or a multifocal MIOL Diffractiva-aA (n = 30) or a bifocal Diffractiva-aA Bi (n = 25), or a monofocal Aspira-aA lens (n = 25), who met the inclusion criteria and were operated at the Department of Ophthalmology, Medical University of Lodz, Poland. After consenting to participate in the study, patients were randomly assigned to one of four groups (3 study groups and 1 comparison group).
The inclusion criteria were the presence of cataracts in both eyes in patients with preoperative best-corrected distance visual acuity (VA) ranging from 0.3 to 0.8 (decimal) and with a corneal astigmatism up to 0.75 Dcyl.
The exclusion criteria were concomitant eye diseases (congenital anomalies of the eyeball, corneal diseases (scars, opacities, preoperative corneal endothelial density below 1,500 cells/mm2), dry eye syndrome, glaucoma, retinal and macular diseases, previous ocular injury, amblyopia, strabismus, uveitis and a history of optic neuropathy, diabetic retinopathy, previous central retinal artery occlusion or central retinal vein occlusion, eyeball tumors), as well as the presence of other diseases that may affect postoperative visual acuity (diabetes, hypertension, stroke, multiple sclerosis, connective tissue diseases). Pregnant and lactating women, as well as professional drivers and pilots were also excluded from the study.
In order to eliminate the bacterial flora of the conjunctival sac before the surgery, all patients were asked to use topical antibiotic drops of levofloxacin 4 times a day for 3 days before the surgery.
All procedures were performed under local anesthesia using topical proxymetacaine drops and lidocaine gel (2%), with additional intracameral anesthesia using 1% lidocaine solution. The procedures were performed by 3 experienced surgeons. In all cases, the pupils were dilated before the surgery using a 1% solution of tropicamide and a 10% solution of phenylephrine.
Patients were operated using the standard phacoemulsification technique through a small 2.2 mm wide clear corneal self-closing temporal incision. After entering the anterior chamber and administering the viscoelastic, continuous circular capsulorhexis (CCC) was performed with microforceps, then two lateral ports (paracenteses) were created with the MVR 20G knife. An infusion fluid – balanced salt solution (BSS) was used to perform hydrodissection. Phacoemulsification was performed using a Stellaris phaco machine (Bausch & Lomb). Cortical masses were removed by irrigation and aspiration. Then, after the viscoelastic had been injected into the anterior chamber, the appropriate lens for the given group was implanted with the use of an injector. Lenses were inserted in group 1 using the Johnson & Johnson UNFOLDER Platinum 1 Series Delivery System injector, in groups 2, 3 and 4 using the MedicelAccuject / Naviject injector. After rinsing the viscoelastic, the corneal wounds were sealed with 0.9% saline (NaCl) solution, without sutures.
After the surgery, all patients used steroid drops with antibiotics containing 3 mg/1 ml of tobramycin and 1 mg/ml of dexamethasone, 4 × daily for 3 weeks, then 2 × daily for 1 week.
All patients were examined before the surgery, on days 1 and 7 after surgery, one month, three and six months after the surgery. The second eye was operated 4-6 weeks after the first one.
Preoperative examination included: assessment of the stage of cataract in the LOCS 3 system, biometry and tests performed during each control: kerato-refractometry, assessment of uncorrected and best corrected visual acuity for distance, intermediate distance (60 cm) and near (40 cm), as well as examination of visual acuity for near with correction for distance, both monocularly and binocularly, examination of the anterior segment and the eye fundus in a slit lamp, tonometry, macular OCT, and measurement of the number of corneal endothelial cells.
During the examinations after in 1, 3, and 6 months, the patients additionally had: contrastometry, assessment of undesirable optical phenomena (halo, glare), the defocus curve, and the questionnaire about the quality of vision and the level of satisfaction after cataract surgery.
RESULTS
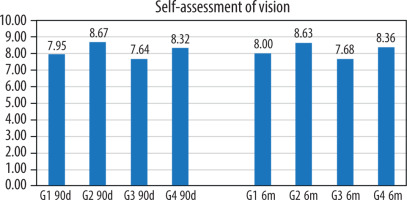
Subjective evaluation of the quality of the patient’s visual functioning was carried out 3 and 6 months after cataract surgery of both eyes using the visual quality questionnaire. The satisfaction turned out to be the highest in group 2 and 4, slightly lower in group 1, and the lowest in group 3 (Figure 1, Table I).
Table I
Statistical significance of differences between the visual quality 6 months after cataract surgery between the study groups
| Group 1 | Group 2 | Group 3 | |
|---|---|---|---|
| Group 2 | > 0.05 | – | – |
| Group 3 | > 0.05 | > 0.05 | – |
| Group 4 | > 0.05 | > 0.05 | > 0.05 |
Statistical analysis on objective assessment of the quality of the patient’s eyesight, carried out 6 months after cataract surgery, showed a significantly lower level of visual quality perception in group 3 as compared to group 2 and 4.
The results of the assessment of visual functioning of patients in all groups, performed 6 months after cataract surgery of both eyes, are shown in Table II. The presence of double vision or duplication of contours was found only in patients from group 4 (4%) and group 3 (4%). Patients from group 3 (16%), group 2 (13.33%), and group 4 (12%) worried about the condition of their eyesight most often, while the patients from group 1 (5%) were the least concerned. The percentage of all activities requiring the use of glasses was> 50% in groups 4, 3, and 1. In other cases, it was < 50%.
Table II
Visual functioning of patients 6 months postoperatively
Assessment of the results of patients’ activities related to near vision, performed 6 months after cataract surgery of both eyes is shown in Table III.
Table III
Assessment of the results of patients’ activities related to near vision
In all patients in group 4, there were difficulties with near-reading (newspapers, small print) or in performing precise tasks (threading a thread) without near-correction, and the need to use glasses in 100% of cases.
In the remaining study groups (1, 2, 3), the number of patients requiring reading glasses was the lowest in group 2 (3.33%), and comparable in groups 1 and 3 (20% each). The number of people who had difficulties with near reading (newspapers, small print) or with performing precise tasks (threading a thread), it was also the lowest in group 2 (6.67%), while it was comparable in groups 1 (25%) and 3 (24% / 28 %). After the use of near correction, the above-mentioned difficulties were resolved in all patients from groups 1, 2, and 3.
Assessment of the results of patients’ activities related to intermediate vision, performed 6 months after cataract surgery of both eyes is shown in Table IV.
Table IV
Assessment of the results of patients’ activities related to intermediate vision
Difficulties with reading the prices of products in the store, were present most frequently in group 4 (60%), and less frequently in groups 1 (10%), 3 (8%), and 2 (6.67%). However, difficulties in finding products in the store on full shelves were noticed only in group 3 in 8.33% of people.
Patients from groups 1 (5%), 2 (3.33%), and 4 (8%) had problems with shaving or make-up. Difficulties with cooking, sewing, and using tools were reported by patients in groups 1 (10%), 2 (3.33 %), and 4 (20%). On the other hand, difficulties in observing the dilator’s reactions were found only in groups 2 (6.67%) and 4 (4%). No patient from any study groups had difficulty recognizing familiar people in the same room.
Ratings of activities related to far vision under photopic conditions 6 months after cataract surgery of both eyes are shown in Table V.
Table V
Activities related to far vision under photopic conditions
Significant difficulties in driving a car in a known area during the day were found in 20% of patients from group 3 who required the use of distance glasses. Difficulties in reading road signs or shop names during the day were found in group 1 (in 8.33% of people). On the other hand, difficulties while watching TV were most frequently found in group 1 (20%), less often in groups 3 (8%), 2 (6.67%) and 4 (4.17%), in addition to eyeglass correction, this activity was most often required by patients from group 1 (10.53%), 4 (8%) and 2 (6.67%).
Rating activities related to far vision in scotopic conditions (at night) 6 months after cataract surgery of both eyes are shown in Table VI.
Table VI
Activities related to far vision in scotopic conditions
Differencesin terms of visual acuity when watching TV with the lights off, it was found most frequently in groups 3 (41.67%) and 1 (35%), less often in groups 4 (14.29%) and 2 (10%).
Difficulty driving a car at night was found in groups 1, 2 and 3 in 33.33% of patients. On the other hand, problems with driving a vehicle in difficult weather conditions were most frequently found in group 3 (57.14%), comparably in groups 2 and 4 (50% each), but less often in group 1 (22.22%).
Presentation of adverse events such as halo, light scattering, and fogging when looking at road signs at night were comparable in groups 1 (33.33%), 2 and 3 (37.5% each), but the rarest – in group 4 (20% ). The phenomenon of glare from opposite-side cars was also most often observed in patients from groups: 2 (70.59%), 1 (41.67%), and 3 (37.50%), and the least frequently – 4 (25%).
Difficulties that patients from groups 1 (10%), 3 and 4 (4% each) had recognition of people or objects after sunset. On the other hand, people from groups 1 (15%), 3 (12%) and 4 (16%) had problems with watching movies in the cinema or theater plays.
The results of the subjective assessment of the patient’s satisfaction level – performed 6 months after the cataract surgery of both eyes using the patient satisfaction questionnaire – are presented in Table VII. The issues included in it concerned, assessment of the ability to function at distance, near and intermediate distances without glasses, the assessment of various everyday activities that require sharp vision at various distances, and the assessment of the patient’s level of satisfaction with their vision.
Table VII
Subjective assessment of the patient’s satisfaction level
Free functioning at a distance without glasses was found in the majority of patients from all studied groups: 2 (86.67%), 3 (84%), 4 (80%), 1 (65%). The others, on the other hand, needed spectacle correction.
The majority of patients from groups 2 (90%), 1 (75%), and 3 (68%) were able to function freely in the near range without glasses. In group IV, 100% of people needed spectacle correction to this distance.
Free functioning up to intermediate distances (50-150 cm) without glasses was observed in the majority of patients from groups 1 (95%), 2 (83.33%), and 3 (76%). In group IV, 100% of people needed eyeglass correction.
Assessment of undesirable optical phenomena 6 months after cataract surgery of both eyes was performed with the help of the patient satisfaction questionnaire, which asked me about the presence of dysphotopsia: halo around light sources, glare (glare), stars (starburst) and the degree of discomfort associated with them.
The presence of a halo around light sources at night 6 months after cataract surgery was most often reported by patients from group 2 (50%), 3 (16%), and 1 (15%), and the least frequently from group 4 (4%). The degree of discomfort associated with visible halos around light sources was generally low and medium in groups: 1 (71.43%), 2 (50%), 3 (44%), 4 (12%), and high – in group 2 (13.33%) and 3 (4%). However, the patients from groups 4 (88%), 3 (52%), 2 (36.67%), and 1 (28.57%) did not experience any discomfort.
The presence of glare (glare) around light sources at night, 6 months after cataract surgery, was reported by patients from group 2 (46.66%), 1 (20%), and 3 (8%). The degree of discomfort associated with visible reflections around light sources was usually low and medium in groups: 1 (71.43%), 2 (56.67%), 3 (40%), 4 (8%), and high – in group 2 (10%) and 3 (4%).
The least frequent side effect was starbursts around light sources at night. The above-mentioned optical phenomenon was often visible in groups 2 (6.67%) and 3 (8%), and less often – in groups 2 (8%) and 1 (5%). The degree of discomfort associated with visible stars around the light sources was low and medium in groups 1 (100%), 3 (16%), and high – in group 2 (6.66%). However, patients from groups 2 (93.33%) and 3 (84%) did not experience any discomfort (Table VIII).
Table VIII
Undesirable optical phenomena 6 months after cataract surgery
DISCUSSION
Hamid et al. [1] 6 months after cataract phacoemulsification with binocular implantation of 3 different lenses: trifocal diffractive IOL AT LISA tri 839 MP (n = 50) and PhysIOL FineVision (n = 50), as well as IOL EDoF Tecnis Symfony ZRX00 (n = 50) – also showed a low frequency of wearing reading glasses. In both MIOL Tri lenses, 100% of patients did not need or have occasional eye glass correction, and 5.6% of people with the Symfony IOL used it frequently. The results of the above-mentioned parameters presented in my work in group 2 are comparable, and slightly higher in group 1.
Monaco et al. [2] analyzed the independence of glasses in 60 patients, 4 months after surgery, cataract extraction with binocular implantation of three different intraocular lenses: EDoF Tecnis Symfony ZXR00 (n = 20), Trifocal Acrysof IQ Panoptix TFNT00 (n = 20) and Monofocal Acrysof SN60WF (n = 20). The authors showed that patients with implanted MIOLs (up to 5%) wore glasses much less often than those who had monofocal IOLs (75%). Independence from glasses to distance was shown by the majority of people with anytype of IOL: Panoptix (90%), Symfony (85%), SN60WF (75%). On the other hand, 100% of patients from both MIOL groups were independent of glasses for intermediate distances, and 15% – from the control group. For near vision, 90% of people with Panoptix IOLs did not need correction, 75% were with Tecnis Symfony, and all patients with monofocal IOLs had to use correction.
Lubinski et al. [3] one year after cataract surgery in 40 patients with bilateral implantation of AtLisa tri 839 MP (n = 20) or TecnisSymfony ZRX00 (n = 20) lenses, showed that 100% of patients with MIOL AtLisa and 90% – with IOL Symfony were independent of glasses. Patients from both groups highly rated their overall visual quality in the VFQ-25 questionnaire: 1.85 ±0.5 and 1.67 ±0.47 in the AtLisa and Symfony groups, respectively. On the other hand, VA results when driving a car during the day, at night or in severe weather conditions were significantly (p < 0.05) statistically better in patients with MIOL AtLisa compared to EDoF Tecnis Symfony.
Webers et al. [4] compared independence from glasses in patients after lens implantation AtLisa tri 839 MP (n = 15) or Tecnis Symfony ZRX00 (n = 15). The authors showed that 3 months after the surgery, 54% of MIOL AtLisa patients and 64% of Symfony IOL patients achieved complete independence from glasses. The percentage of patients who did not need glasses at all or who only had to wear them 1 hour a day was 85% for the MIOL AT LISA group and 79% for the IOL Symfony group, respectively. Vision-related quality of life was comparable in both groups. The above mentioned results are very similar to those reported in my study where 70% of the patients with the Tecnis Symfony IOL and 97% with the MIOL Diffractiva-aA were completely independent of the glasses or wore them very rarely, and the VA quality was also comparable.
Dexl et al. [5], 6 months after cataract surgery of 24 patients with MIOL implantation (Diffractiva-aA), analyzed patients’ responses from the satisfaction questionnaire. The authors noted that no patient reported serious difficulties with any of the assessed lifestyle activities. Independence from glasses was admitted by the majority of patients (91.6%), and only some patients (4.2%) required near and distance correction. The researchers also showed high satisfaction with the procedure admitted by 91.7% of patients (the remaining 8.3% were also moderately satisfied). The results of reported functional difficulties, independence from spectacle correction and patient satisfaction presented in our study were similar in group 2.
Comparable results of independence from glasses were reported by Kohnen et al. [6] after bilateral MIOL Acrysof IQ ReSTOR SN6AD1 implantation (with add +3.00 D) in a large multicentre study with 93 patients, 88% of whom were completely free from correction; 99% of patients did not have glasses for distance or occasionally wore them, 94% – for intermediate distances, and 89% – for near distances.
Schrecker et al. [7] one year after cataract surgery with binocular MIOL Diffractiva-aA implantation assessed the satisfaction of patients with far and near VA without ocular correction under various lighting conditions. The obtained results of independence from distance glasses indicated a high satisfaction of 100% of people during the day and 60% – at night (the remaining patients were satisfied (20%) or moderately satisfied (20%)). On the other hand, independence from reading glasses in daytime conditions with high satisfaction was presented by 90% of people (the remaining 10% were satisfied), and in twilight conditions – 70% (the rest – moderately satisfied). We describe very similar results.
Grabner [8] examined results of cataract extraction with binocular MIOL implantation 3 months after the Diffractiva-aA+3.5D implantation (group 1, n = 30) or MIOL AcrySof Restor +3.0 D (group 2, n = 30) – they also showed small frequency of wearing glasses in both groups with slightly better results in the Diff-aA group. MIOL patients with Diffractiva-aA occasionally used corrective glasses in 15% of cases, and patients with MIOL AcrySof Restor – in 29% of cases. The authors also showed that in conditions of low light or worse contrast, the visual performance of Diff-aA is better than that of AcrySof Restor, which may be related to the level of chromatic aberration of the materials of these lenses: respectively higher in 1 lens (57 Abbe), and lower – in 2 (37 Abbe).
Chitkara et al. [9] also analyzed the quality of life outcomes of people after binocular Diffractiva-aA IOL implantation. The authors showed that all patients functioned comfortably without near and intermediate distance glasses. Only one person (with VA 20/20), despite the lack of correction, reported difficulties with distance vision. Independence from glasses was reported by 93% of patients, the remaining 7% needed occasionally spectacle correction. In my study, the results in group 2 were very similar.
Rasp et al. [10] presented the 6-month study results after binocular MIOL Diffractiva-aA implantation in 17 patients (34 eyes). It turned out that 93.3% of patients never wore glasses and the remaining 6.7% used them rarely. These results are similar to those obtained in our group 2.
Farvardin et al. [11] one year after cataract surgery with MIOL binocular implantation of AlconAcrysof IQ Pan-Optix TNFT00 (n = 20) or TecnisSymfony ZXR00 lenses (n = 20) presented the VA quality results. The near vision results turned out to be significantly higher in the MIOL TNFT00 group (86.6%) than in the EDoF ZXR00 group (65.5%) (p = 0.001 and p = 0.015, respectively). Satisfaction with VA for distance, color vision, independence from glasses was slightly higher in patients with IOL PanOptix, while patients with Tecnis Symfony were more satisfied with VA while driving and with their peripheral vision.
The occurrence of undesirable optical phenomena of the halo type around light sources, glare, and starbursts can have an adverse effect on the post-operative quality of a patient’s vision in mesopic conditions. An equally important issue is to determine the degree of discomfort associated with these phenomena.
The presence of a halo around light sources at night, 6 months after the surgery was most often reported by patients from group 2 (80%), 3 (56%), 1 (35%), and the least frequently from group 4 (12%). The degree of discomfort associated with the visible phenomenon was usually low and medium in groups: 1 (71%), 2 (50%), 3 (44%), 4 (12%), and high – in groups 2 (13%) and 3 (4%). Nevertheless, in all groups there were patients who never experienced any discomfort (29% in group 1, 37% in group 2, 52% in group 3 and 88% in group 4).
The occurrence of starburst around light sources at night, 6 months after cataract surgery, was reported by patients from groups 3 (16%), 2 (7%) and 1 (5%). It was the least frequent photo-optical phenomenon.
The degree of discomfort associated with the visible star-burst effect was generally low or medium in most groups. The majority of patients in each group were satisfied with their eyesight. The majority of patients from all groups expressed the willingness to implant the same lens.
Hamid et al. [1] 6 months after phacoemulsification with binocular implantation of 3 different lenses: trifocal diffractive IOL AT LISA tri 839 MP (n = 50) and PhysIOL Fine Vision (n = 50), as well as IOL EDoF Tecnis Symfony ZRX00 (n = 50) assessed undesirable optical phenomena of the halo and glare types. The presence of the above-mentioned phot-optic phenomena of a moderate or high degree were present in 20% of patients with IOL ATLISA and Fine Vision, while it caused problems only in 5.6% of patients with IOL Symfony. The authors also noted high satisfaction in 94.4% of patients with IOL Symfony and 93.3% of patients with ATLISA, these patients would choose the same lens again or would recommend this IOL model to their friends and family. On the other hand, the dissatisfaction rate was higher in the patients with FineVision IOL.
The results of the above-mentioned parameters presented in my work in groups 1 and 2 are comparable.
Glare was observed in up to 63.6% of patients by different researchers in their studies evaluating other types of diffractive MIOLs (Acrysof IQ ReSTOR SN6AD1, Acri. LISA 366 D, AcrivaReviol MFM 611, Tecnis ZMA00).
Schrecker et al. [7] assessed the undesirable halo and glare optical phenomena one year after cataract surgery with binocular MIOL Diffractiva-aA implantation and found that it occurred in 70% of patients. A low degree of discomfort was reported by 86% of people and a moderate degree of discomfort by 14% of patients. All patients quickly got used to the above-mentioned optical phenomena and said they would have the same lens implanted. The results of the above-mentioned the parameters presented in my work in group 2 are very similar.
Monaco et al. [2] analyzed side effects in 60 patients 4 months after cataract extraction with binocular implantation of three different intraocular lenses: EDoFTecnis Symfony ZXR00 (n = 20), Trifocal Acrysof IQ Panoptix TFNT00 (n = 20) and Monofocal Acrysof SN60WF (n = 20). The halo effect was the most common symptom in both multifocal IOL groups. Researchers found that approximately 95% of Symfony IOL patients experienced the halo effect, i.e.: 25% observed it very often, and 20% experienced severe discomfort. Glare and starburst were also common photo-optical phenomena in both groups of multifocal lenses. The appearance of glare was noticed in 90% of patients with IOL EDoF and as much as 12% felt discomfort. In the present study, a smaller number of people (35%) with IOL Symfony noticed halos and glare and the degree of discomfort associated with them was low to medium.
Farvardin et al. [11] one year after cataract surgery with binocular implantation of Alcon Acrysof IQ PanOptix TNFT00 (n = 20) or Tecnis Symfony ZXR00 lenses (n = 20) found no glare in case of MIOL and EDOF IOLs in 45% and 58.3% of people, respectively (p < 0.05), and no halos in 57% and 65%, respectively.
Lubinski et al. [3], in 40 patients with bilateral implantation of AtLisa tri 839 MP (n = 20) or Tecnis Symfony ZRX00 (n = 20) lenses, showed one year after cataract surgery that the frequency of the halo effect and the level of discomfort associated with it were significantly (p = 0.000) higher in the MIOL AtLisa group (20%, 2.5 ±0.53) compared to the IOL Symfony (5%, 0, 89 ±0.13). Glare was also significantly (p = 0.000) less perceived by patients with Symfony IOL (5%, 0.5 ±0.69) compared to patients with MIOL AtLisa (20%, 2.5 ±0.53).
Webers et al. [4] analyzed the occurrence of photo-optical phenomena in patients after AtLisa tri 839 MP (n = 15) or Tecnis Symfony ZRX00 (n = 15) lens implantation. The authors showed that 3 months after the surgery, 43% of EDoF Symfony patients and 15% of AT LISA IOL patients did not experience the “halo” effect (p = 0.12). On the other hand, the occurrence of halo causing discomfort was reported more frequently in patients with AT LISA IOL (39%) compared to patients with Symfony IOL (21%) (p = 0.33). In addition, the researchers found that 50% of people with EDoF Symfony and 69% with AT LISA IOL did not see the glare effect, and only in 7% and 8% of patients, respectively, the glare caused discomfort (p = 0.96). The authors also noted high satisfaction among these patients – 93% of patients with IOL Symfony and in 92% of patients with AT LISA would choose the same lens again or recommend this model to their friends and family. In the above-mentioned study, no halo was seen by a higher number of people with IOL Symfony (65%) and MIOL AT Lisa (20%). No-glare was also observed in the Symfony group (65%) and less frequently in the MIOL Diffractiva group (24%). Patients noticing the halo and glare effects – with EDoF IOLs did not feel discomfort, and those with diffractive MIOLs felt discomfort in about 10-13% of cases.
Dexl et al. [5] evaluated results of 24 patients with Diffractiva-aA MIOL implantation and analyzed the side effects reported by patients 6 months after cataract surgery. The authors noted that most patients (58.3%) did not experience or were not disturbed by halos at night, 25% felt small discomfort, 12,5% felt medium degree of discomfort, while 4.2%experienced a high degree of discomfort. Glare occurred in 4% of patients to a moderate degree. The results of the reported halo effect in patients presented in my study were similar.
Grabner [8] 3 months after cataract extraction with binocular MIOL Diffractiva-aA+3.5 D implantation (group 1, n = 30) or MIOL AcrySof Restor +3.0 D implantation (group 2, n = 30) also showed high patient satisfaction in both groups and found that none of the respondents was dissatisfied with their cataract surgery.
Chitkara et al. [9] also assessed the occurrence of undesirable halo and glare optical phenomena one year after cataract extraction with binocular Diffractiva-aA IOL implantation. Most patients (79%) did not experience any halos at night or were not disturbed by them. Glare from headlights did not bother or was not noticed in 90% of people. Only in 2 patients the above-mentioned photo-optical phenomena caused difficulties in everyday activities. Despite the occurrence of the undesirable phenomena, patients had a high level of satisfaction with cataract surgery. In my study, the appearance of photo-optical effects and patient satisfaction after surgery in group 2 were at a similar level.
Rasp et al. [10] presented the six-month study results after the binocular MIOL Diffractiva-aA implantation in 17 patients (34 eyes). It turned out that 53% of people have never seen a halo effect at night, 13% have seen it from time to time, 27% have seen it very often, and 7% could always see it. In case of glare phenomenon present at night, 80% of patients have never noticed it, 7% have rarely seen it, 3% could see it from time to time, and 10% could see it very often. Importantly, none of these patients reported any serious concerns about the visible photo-optical phenomena. Moreover, all patients stated that they were satisfied and 87% of them were very satisfied with their vision. The percentage of patients who reported halo and glare effects in patients from my work was higher, while the satisfaction with the entire procedure was at a similar level.
The potential limitation of this study is a relatively small number of patients (25-30 patients in each group), which resulted from a limited number of the intraocular lenses used in the study. Therefore a further research with a higher number of recruited patients would address this issue and would be valuable.
CONCLUSIONS
Undesirable optical phenomena such as halo and glare occurred most often in patients with diffractive-refractive multifocal lenses, were less severe in groups with extended depth of focus lenses and diffractive-refractive bifocal lenses, and were the least frequent in patients with monofocal lenses.
The majority of patients from all groups were highly satisfied with their eyesight after cataract surgery, although a slightly lower percentage was observed in the group with monofocal lenses.
The percentage of patients who would decide to undergo the surgery with the same lens again was very high and similar in all groups.
The quality of life related to vision was rated as the highest by patients from groups with diffractive-refractive multifocal lenses and with monofocal lenses, it was slightly lower in patients with extended depth of focus lenses, and it was the worst in patients with bifocal diffractive-refractive lenses.

 POLSKI
POLSKI