INTRODUCTION
Ocular trauma is a leading cause of blindness, particularly in young adult males, with approximately 55 million eye injuries reported globally each year [1]. Open globe injuries (OGIs), characterized by full-thickness wounds of the eye wall, are a significant contributor to blindness and visual impairment, with an estimated 203,000 cases annually worldwide [2]. Despite the prevalence of ocular trauma, protective eyewear is rarely used, with only a small percentage of patients reporting its use during accidents [3]. Studies have shown that a significant number of OGIs are work-related, and these injuries often result in severe visual impairment. Penetrating injuries with intraocular foreign bodies (IOFBs) account for a substantial portion of eye injuries, predominantly in men and often resulting from workplace accidents, especially those involving metal tools [4]. Such foreign bodies can lead to both partial and full-thickness ocular injuries, sometimes affecting the posterior segment of the eye.
Accurate diagnosis and prompt treatment are crucial, and a thorough clinical examination, including slit lamp evaluation and imaging techniques such as ultrasonography and computed tomography (CT), plays an essential role in determining the appropriate course of action [5, 6].
We present a rare case of a patient with a scleral injury, maintaining full visual acuity, caused by a metallic object that penetrated the eye and was subsequently spontaneously removed from the eye due to a reflex action as the patient moved away from the source of the injury.
CASE REPORT
A 21-year-old patient was referred to the ophthalmic casualty after sustaining an injury to his left eye at work without protective glasses. He was cutting a sheet of metal with metal shears, which, under the tension generated, recoiled toward the patient’s face and pierced the lower eyelid nasally, passing through its entire thickness, as well as through the palpebral and bulbar conjunctiva and the superonasal part of the sclera. On examination, visual acuity was not reduced, and the intraocular pressure was 16 mmHg. During the slit lamp examination, a conjunctival wound was observed at 7 o’clock.
Initially, the presence of an intraocular metallic foreign body was suspected.
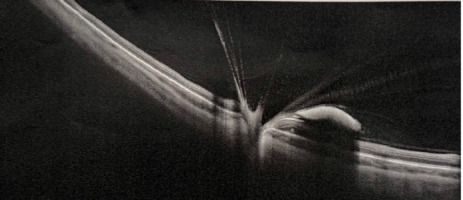
Examination of the anterior segment of the eye revealed no abnormalities in the cornea, a clear anterior chamber with no signs of Tyndall effect, a transparent lens, and preserved visibility of the fundus. Fundoscopic examination revealed the optic disc (n. II) with clear borders, the macula with a reflex, vitreous hemorrhage, a full-thickness wound of the eye wall at 10 o’clock surrounded by small hemorrhages, local retinal detachment, and hemorrhagic opacities in the nasal quadrants hindering the assessment of the retina (Figure 1). In the ultrasound examination of the left eyeball, a hemorrhage into the vitreous body was visualized (Figure 2).
Figure 1
Fundoscopic examination of the left eye on the day of admission. Vitreous hemorrhage, a scleral wound at 10 o’clock surrounded by small hemorrhages, local retinal detachment, and hemorrhagic opacities in the nasal quadrants, hindering the assessment of the retina. A) Superior and inferior nasal quadrants of the left eye. Hemorrhagic opacities in the nasal quadrants. B) Superior and inferior temporal quadrants of the left eye
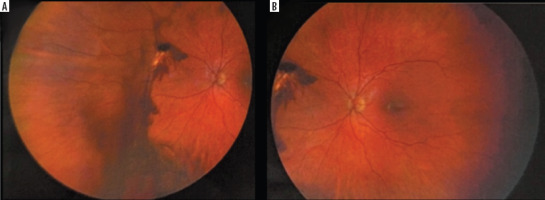
Figure 2
A, B. Ultrasound B-scan examination of the left eye on the day of admission, vitreous hemorrage is indicated by red arrows
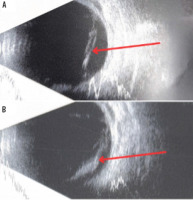
Computed tomography scan of the orbits ruled out the presence of an intraocular metallic foreign body (Figure 3). Pointed areas of increased density were visible in the sclera (at the junction with the cornea) and the vitreous body of the left eye, indicating post-traumatic changes with blood strands.
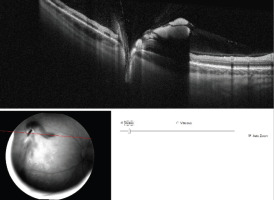
Figure 3
Optical coherence tomography examination of the left eye on the day of admission, showing the site of retinal injury with vitreoretinal junction and disruption of the neurosensory retina was visualized
The procedure was performed under local anesthesia, involving a revision of the wounds in the palpebral and bulbar conjunctiva, as well as the sclera on the nasal side. The conjunctival, scleral and lower eyelid wound edges were sutured with 8.0 sutures. Laser photocoagulation was performed around the wound. During the 7-day hospitalization, the patient was given cefuroxime intravenously at a dose of 1,500 mg and sulfamethoxazolum + trimethoprimum intravenously at a dose of 80 mg + 16 mg, on the first and last day once a day and twice a day on the remaining days. On days 2, 3, and 4, methylprednisolone was administered intravenously at a dose of 500 mg; on subsequent days until the end of hospitalization, the dose was reduced to 250 mg. The above drugs were given once a day.
Postoperative visual acuity was 5/5 binocularly with IOP measurements 15 mmHg in OD and 16 mmHg in OS. During the follow-up visit, one month after the procedure, a comparative image was taken during the fundoscopic examination of the left eye (Figure 4), and an OCT examination of the left eye was also performed (Figure 5).
DISCUSSION
Ocular trauma is the main cause of blindness in the teenage and young adult male population, which makes it a very important topic that needs to be carefully analyzed. Our patient’s case concerns an OGI, which we can divide according to the location of the wound on the ocular surface. In OGIs, we can distinguish a Zone I wound, which is confined to the cornea, a Zone II wound, which extends into the anterior 5 mm of the sclera, and a Zone III wound that affects the sclera more than 5 mm away from the limbus [7].
Penetrating eye injuries involving an intraocular foreign body account for 18% to 41% of all eye injuries [3]. Intraocular foreign bodies are predominantly found in men, who comprise 92-100% of the affected population [3, 4, 8]. Workplace accidents are the leading cause of such injuries, occurring in 54% to 72% of cases. High-risk activities typically involve the use of metal tools, such as chiseling, hammering, and drilling, which account for 60-80% of incidents where a foreign body enters the eye [4, 8]. Foreign bodies that penetrate the ocular coat can cause either partial or full-thickness injuries to the cornea and sclera, potentially involving the posterior segment [8].
Only 3-5,5% of patients suffering from penetrating eye injuries reported wearing protective eyewear at the time of the accident [3].
Injuries such as scleral and limbal lacerations can result from sharp objects like scissors, thorns, iron nails, fish hooks, and wood fragments. A thorough and precise slit lamp examination is essential to identify conditions such as sclerolimbal tears, occult globe ruptures, posterior scleral tears, intraocular foreign bodies, corneal infiltrates, endophthalmitis, and panophthalmitis. Scleral and limbal lacerations are a type of open globe injury that can lead to significant vision loss. Clinical signs include conjunctival congestion, subconjunctival hemorrhage, partial or full-thickness disruption of the sclera or corneal limbus, iris prolapse, pupil peaking, and breaches in the anterior lens capsule. Vitreous prolapse may also occur, but is not always present. The presentation varies between cases, and diagnosis is primarily based on clinical evaluation [9].
TWO PATHS: PRESENCE OR ABSENCE OF INTRAOCULAR FOREIGN BODY?
Regardless of the presence or absence of an intraocular foreign body, proper management of a patient who has suffered an open eye injury is extremely important.
The ophthalmologist’s responsibilities include obtaining a detailed yet focused medical history, evaluating the visual acuity of each eye, conducting an external inspection, performing an examination with a slit lamp and a 90 D lens, carrying out ophthalmoscopy, and utilizing ultrasonography when appropriate. However, ultrasonography may be avoided if a large anterior wound is present, the patient is uncooperative, or the ophthalmologist is not experienced with the procedure [5]. Additionally, CT should be considered unless all necessary details of the trauma are already clear, keeping in mind both medical and legal implications [6]. Magnetic resonance imaging (MRI) may be used if detailed orbital soft-tissue evaluation is required, provided there is no metallic intraocular foreign body (IOFB).
In general, wound suturing can be postponed for about a day if necessary. However, delaying wound closure carries certain risks, including expulsive hemorrhage and endophthalmitis [5]. For this reason, it is recommended to close the wound as promptly as possible.
PROGNOSTIC FACTORS IN CORNEO-SCLERAL LACERATIONS
Recent advancements in understanding injury mechanisms, technological progress in diagnostic methods, and widespread access to reconstructive techniques have significantly improved the prognosis of severe eye injuries in developed countries. According to a statistical analysis by Kuhn et al., based on data from the United States Eye Injury Registry, the incidence of monocular blindness following severe eye injuries is now reported to be less than 10% [10].
The time elapsed since the injury and the severity of the damage largely determine the visual outcome until appropriate surgical treatment is performed [7]. Patients should not be given unrealistic expectations about their visual recovery until a thorough evaluation is completed, especially after surgery. Factors such as an initial visual acuity of 20/200 or better, a wound length of 10 mm or less, an anterior wound location extending to the plane of the four rectus muscles, and a sharp mechanism of injury are indicative of a potential for excellent final visual acuity (20/60 or better). On the other hand, predictors of poor visual outcomes include an initial visual acuity of light perception or no light perception, a wound length greater than 10 mm, and wounds caused by blunt or missile objects that extend beyond the insertion planes of the rectus muscles. Although globe rupture and injury to the posterior segment often lead to significant visual impairment, advances in diagnostic techniques, surgical methods and rehabilitation have improved visual outcomes in many cases [8].
Corneal lacerations due to sharp objects have a better prognosis compared to blunt trauma injuries [7].
BACTERIAL ENDOPHTHALMITIS – HOW TO AVOID IT?
Bacterial endophthalmitis remains a significant potential complication in patients with OGIs following surgical repair, often leading to worse visual outcomes. To mitigate this risk and improve postoperative vision, perioperative and postoperative antibiotic administration is a standard practice [11]. Several factors increase the likelihood of postoperative endophthalmitis in open globe injuries, including delays in surgical repair, the presence of retained IOFBs, and rupture of the lens capsule [11]. Research has shown comparable rates of postoperative endophthalmitis when using systemic intravenous (IV) antibiotics versus oral antibiotic regimens [12].
To evaluate different strategies for preventing endophthalmitis after the surgical repair of traumatic OGIs, Fell et al. conducted a survey [13]. They found that 90% (27/30) of the participating programs used perioperative intravenous (IV) antibiotics, with 78% (21/27) of these administering a single dose. Intraoperatively, 27% (8/30) of programs used intravitreal antibiotics, while 60% (18/30) administered subconjunctival antibiotics. Postoperative care included topical antibiotics in all programs (100%, 30/30) and topical steroids in 97% (29/30). However, only 53% of respondents prescribed oral antibiotics at discharge. Among the three programs that did not use IV antibiotics, all opted for intravitreal therapy, with one also prescribing oral antibiotics after discharge. The findings highlight a general preference for a single preoperative IV antibiotic dose, varied intraoperative antibiotic regimens, and universal use of postoperative topical antibiotics. This variability points to the need for a randomized comparative study to define the best standard of care for managing these patients [13]. Moreover, tetanus prophylaxis should be considered following perforating or penetrating globe injuries, especially if the patient’s immunization status is unknown or not current. Additionally, tetanus immune globulin may be given based on the specifics of each case [7].
LONG-TERM COMPLICATIONS AFTER OPEN GLOBE REPAIR
Late complications after surgical management of trauma include mechanical complications such as glaucoma, epiretinal membranes, post-traumatic cataracts, vitreoretinal proliferations, retinal breaks, or tractional retinal detachment. Chemical complications include calcification and siderosis, and in addition to these, inflammation or atrophy of the eyeball can occur [14]. The etiology of secondary traumatic complications, analogous to primary complications, can be mechanical, chemical, or inflammatory. There is no clear position in the literature on the incidence of late injuries of mechanical origin, but the most commonly described complications include post-traumatic cataract (15-57%), retinal detachment (11-46%) and the development of vitreoretinal proliferations (15-25%) [3, 14-18]. As for traumas of chemical etiology, they occur in injuries with the presence of metallic foreign bodies, the most common pathologies being calcification and siderosis. The time at which these complications occur is usually distant from the time of injury, and depends on whether the foreign body was successfully removed or if it was done with a long delay. These complications usually appear a few weeks or months after the accident, but can occur even a few years after the injury [14].
CONCLUSIONS
Early diagnosis and prompt surgical or pharmacological intervention can, in many cases, save a patient’s vision and carry satisfactory results in improving patients’ quality of life. For these reasons, public education about first aid for eye injuries and providing rapid access to specialized care are of great importance. Employers should ensure that employees are equipped with appropriate protective eyewear and are educated on its correct usage. This approach can help lower the occurrence of eye injuries and minimize their severity when they do occur.

 POLSKI
POLSKI