INTRODUCTION
Primary open angle glaucoma (POAG) may present in an advanced stage of the disease [1] mandating urgent treatment and low target intraocular pressure (IOP) [2]. Treatment options include angle lasers [3], medical treatment [4] and surgical treatment. A number of surgical procedures are at the disposal of the treating ophthalmologist, including filtering surgery [5], angle surgery [6], and combination procedures [7], among others, with each surgical option coming along with its unique set of complications. Here we present a case of POAG managed by combined trabeculotomy-trabeculectomy with mitomycin that developed localised haemorrhagic Descemet detachment during the trabeculotomy that resolved into a localised sub-Descemet haemosiderin deposit.
CASE DESCRIPTION
Clinical course
A 56-year-old male presented to the ophthalmology outpatient department of Alexandria Main University Hospital complaining of a diminution of vision in the left eye. Complete ophthalmic examination revealed a best corrected visual acuity (BCVA) of 0.5 (OD) and hand motion (HM) (OS), a manifest refraction of cylinder –0.75 × 95° (OD) and –7.50 cyl –1.25 × 70° an intraocular pressure (IOP) of 22 mmHg (OD) and 30 mmHg (OS), clear lenses, cup/disc ratios of 0.5 (OD) and 0.9 (OS) and gonioscopically open angles (Shaeffer grade 4; OU). Humphrey visual field (HVF) revealed for the right eye a mean deviation (MD) of –1.89 dB, a pattern standard deviation (PSD) of 2.68 dB, a visual field index (VFI) of 96% and a glaucoma hemifield test (GHT) that was outside normal limits. HVF was unreliable for the left eye. A diagnosis of primary open-angle glaucoma (POAG) was made, and the patient was prescribed topical IOP-lowering therapy comprising prostaglandin analogues (PGAs; OU), a combination of carbonic anhydrase inhibitors (CAIs) – β-blocker combination, and topical brimonidine (OS). Subsequent follow-up demonstrated IOPs of 12 mmHg (OD) and 20 mmHg (OS), and hence the target IOP (set in the early teens) was not achieved in the left eye. The patient was counselled about the need for surgical intervention to lower the IOP in the left eye, and a decision to perform a combined trabeculotomy-trabeculectomy with mitomycin C was considered.
Surgical procedure
Exposure of the operative field started with a corneal traction suture and a corneal paracentesis, which were followed by a fornix-based conjunctival incision. Mitomycin C in a concentration of 0.04% was applied using a soaked microsponge applied to the scleral surface for 1 minute and was thoroughly rinsed. A partial thickness triangular scleral flap measuring 4 × 4 × 4 mm, half of the scleral thickness was dis sected forward 2 mm into the clear cornea. Radial incisions at the surgical limbus were performed till exposure of Schlemm’s canal, and a Neuhann (Geuder instruments) metal trabeculotome was used to perform the trabeculotomy. The trabeculotome was introduced into Schlemm’s canal on the nasal (right) side of the incision and swept towards the anterior chamber (AC) to perform the trabeculotomy, which was uneventful. The trabeculotome was then introduced into Schlemm’s canal on the temporal (left) side of the incision and swept towards the AC to perform the trabeculotomy. Upon withdrawal of the trabeculotome from Schlemm’s canal a rounded red localized lesion (drop of blood) accumulated gradually in the depth of the substance of the cornea (accumulating in a plane superior to the iris and the AC); the intracorneal location of the red lesion was confirmed by absence of blood in the AC upon irrigation of the AC. The performance of a trabeculectomy and a peripheral iridectomy completed the surgery. Closure of the scleral flap was achieved by 3 releasable sutures, which were followed by closure of the conjunctiva with 10/0 nylon mattress sutures. Surgery was concluded by subconjunctival injection of atropine and dexamethasone and eye patching.
Postoperative follow-up
Day 1 examination revealed a dark red, rounded drop of blood in the supertemporal quadrant of the cornea in the sub- Descemet plane (between the corneal stroma and the Descemet membrane), not encroaching on the pupil border (Figure 1). An Anterior segment optical coherence tomography (AS-OCT) confirmed the location of the blood (Figure 2). The BCVA was still HM (the same as preoperatively), the bleb was pale, diffuse, and low, and the fundus demonstrated flat retina and flat choroidals with a C/D ratio of 0.9 (as preoperatively). The patient was instructed to instill the postoperative topical medications and maintain follow-up. Subsequent follow-ups over several months revealed gradual depigmentation of the sub-Descemet blood transforming into a yellow colour while retaining the same size (Figure 1). After 1 year of follow-up examination revealed a BCVA of 0.5 (OD) and 0.12 (OS), a manifest refraction of cylinder –0.75 × 95° (OD) and –6.0 cyl –4.0 × 115° an IOP of 12 mmHg (OD) and 10 mmHg (OS), clear lenses, cup/ disc ratios of 0.5 (OD) and 0.9 (OS) and a pale, diffuse, low bleb (OS). The localised sub-Descemet haemosiderin deposit remained stationary until the final follow-up.
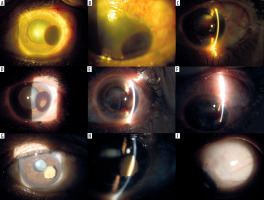
Figure 1
Composite demonstrating the slit lamp photos of the operated eye. The top row demonstrates the appearance of the eye on day 1 postoperatively. A) Diffuse illumination photo demonstrating localised haemorrhagic Descemet detachment. B) Diffuse illumination photo with the eye looking down, demonstrating the operative site and the early filtering bleb. C) Optical section photo demonstrating the sub-Descemet location of the localised haemorrhage. Middle row demonstrating the appearance of the eye 5 months postoperatively. D) Diffuse illumination photo demonstrating localised haemorrhagic Descemet detachment with starting a localised area of haemoglobin breakdown into haemosiderin with evident localised colour change. E) Optical section photo demonstrating the sub-Descemet location of the localised haemorrhage with the area of haemosiderin in the centre. F) Oblique illumination photo with the eye looking down, demonstrating the operative site and the filtering bleb. Bottom row demonstrating the appearance of the eye 1 year postoperatively. G) Diffuse illumination photo demonstrating localised lesion of haemosiderin deposited beneath the Descemet detachment. H) Optical section photo demonstrating the sub-Descemet location of the localised haemosiderin deposit. I) Oblique illumination photo with the eye looking down, demonstrating the operative site and the filtering bleb
DISCUSSION
This is a case of advanced uncontrolled POAG in an adult that was managed by combined trabeculotomy-trabeculectomy with mitomycin C and developed a localised sub-Descemet bleeding as a complication of the second (temporal) trabeculotomy after a successful first (nasal) trabeculotomy. Initial scrutiny of the patient clinical data demonstrates that the patient presented to ophthalmic care at a significantly advanced stage of the disease. This highlights the importance of raising awareness about the generally asymptomatic nature of the early disease and the need for effective screening programs, as already highlighted by previous reports [8]. The fact that the patient suffered unilateral (left) high myopia raises the possibility of anisometropic amblyopia in the afflicted left eye, hence providing further explanation for the reason why progressive deterioration of visual function in that eye by the POAG that remained unnoticed by the patient. The generally asymmetric nature of POAG (as reported [9]) is evident by the relatively good result of the right visual field. In this patient, although medical treatment brought about a reduction of the IOP, this reduction was judged to be insufficient to prevent further deterioration of the optic nerve and visual function, and the decision to perform surgery was taken. This need for a low target IOP in cases of advanced glaucoma is in accordance with other reports [2]. The decision to perform a combined trabeculotomy-trabeculectomy (with mitomycin C) was based on recent reports [7] citing the efficacy and relative safety of combined angle and filtering procedures in adult glaucoma. The procedure of ab-externo trabeculotomy includes, after cannulation of Schlemm’s canal by a metal probe, an inward sweep of the trabeculotome into the AC, thus cutting through the inner wall of Schlemm’s canal (SC) and the trabecular meshwork (TM). This step requires some resistance to the trabeculotome to cut, rather than dissect through, the tissues. This resistance is offered by a full tension of the closed formed globe for the first trabeculotome pass (in this the case the in the nasal direction). After the nasal trabeculotomy the tension dropped and this was not compensated for by the surgeon. The result was low resistance offered to the second trabeculotome pass (in this case the temporal) and hence the result was blunt dissection into the tissues (rather than cutting through inner wall of SC and TM) and hence detachment of the Descemet membrane from the overlying corneal stroma (given that this the anatomical plane of SC; the corneal endothelium and Descemet membrane continue to form the TM endothelium and trabeculae). The trickle of blood was the consequence of the negative pressure created by the Descemet detachment and the reflux of blood into SC (as a consequence of globe decompression to below the episcleral venous pressure by the nasal trabeculotomy). The fact that the surgeon made the trabeculotomy sweep rather limited was responsible for the Descemet detachment (and hence the accumulated blood) being localized and spared the pupil (and hence did not directly obscure vision). The authors hypothesise that this complication could be avoided by adequate pressurization of the globe (by injecting fluid or viscoelastic through a preplaced paracentesis) after the first trabeculotomy pass and before the second trabeculotomy pass. This build-up of pressure may provide the resistance necessary for the trabeculotomy to cut (rather than dissect through) the tissues. Haemorrhagic Descemet membrane detachment has been previously reported by Djavanmardi et al. [10] and Fujimoto et al. [11] in association with glaucoma surgery (non-penetrating glaucoma surgery associated with needling), Najjar et al. [12] (trauma) among others [13-15]. In contrast to these reports, the Descemet detachment in this case was localised, did not lead to corneal staining, did not require surgical evacuation and did not resolve completely but left behind a residual sub-Descemet haemosiderin lesion.
The fact that the blood accumulation in the sub-Descemet plane was a trickle rather than an active bleeder accounted for the lesion remaining localized and not progressive in the postoperative period. The depigmentation into the yellow colour is a natural consequence of haemoglobin breakdown [16]. Given that BCVA was not affected and the IOP was under control, up to 1 year of follow-up justified the decision of follow-up and “wait and see” for the localized lesion. Whether the mild increase in the cylinder at 1 year was a consequence of corneal distortion from the sub-Descemet lesion is a matter of speculation (since no studies of corneal topography were performed before or after the glaucoma surgery). In contrast to other reports of haemorrhagic Descemet membrane detachment, no corneal staining was noticed in this case. The relatively small size of the bleed may have been responsible for sparing the cornea. To the best of the authors’ knowledge, this is the first report of localised Descemet detachment complicating trabeculotomy in a case of POAG and ending in a localised haemosiderin deposition in the sub- Descemet plane.
CONCLUSIONS
The haemorrhagic Descemet detachment may complicate combined trabeculotomy-trabeculectomy with mitomycin C for POAG, which may end up in a localised sub-Descemet haemosiderin deposit. Keeping the globe and the AC pressurized at all times during the surgery and especially before the trabeculotome sweeps into the AC may help avoid this complication.

 POLSKI
POLSKI




