INTRODUCTION
The problem of hypertension affects about 10% of pregnant women worldwide. It is associated with an increased risk of morbidity and mortality, both for the mother and the child. Hypertensive disorders of pregnancy (HDP) include preeclampsia, eclampsia, preeclampsia superimposed on chronic hypertension, hypertension, and pregnancy-induced hypertension (PIH). Preeclampsia is a pregnancy complication affecting about 2-8% of pregnant women in the world [1]. It is characterized by increased blood pressure (> 140/90 mmHg), proteinuria (> 300 mg/24 h) and peripheral oedema. It usually occurs after 20 weeks of pregnancy [2]. It may also occur intrapartum and postpartum. Severe preeclampsia is characterized by blood pressure values higher than 160/110 mmHg, proteinuria (≥ 2 g/24 h), increased creatinine level (> 2 mg/dl), oliguria, thrombocytopenia, epigastric pain, central nervous system disorders, vision disorders, headache, pulmonary oedema, and increased level of hepatic enzymes. The occurrence of tonic-clonic seizures or coma together with the aforementioned symptoms means that the condition has turned into eclampsia. In 4-20% of cases, patients with pre-eclampsia develop its more severe form – HELLP (hemolysis-elevated liver enzymes-low platelets) syndrome, characterized by a triad of symptoms: haemolytic anaemia, increased level of hepatic enzymes, and thrombocytopenia. The problem affects 0.5-0.9% of all pregnant women, mainly during the third trimester, and less frequently within the first week after delivery [3]. Female mortality associated with the occurrence of HELLP is 1-25%, and perinatal mortality of the child is 7.4-34% [3].
Vision disorders secondary to preeclampsia occur in 25-50% of patients [4]. One of the causes of deteriorated vision in diseases involving hypertension during pregnancy is bullous, serous retinal detachment (SRD).
CASE REPORT
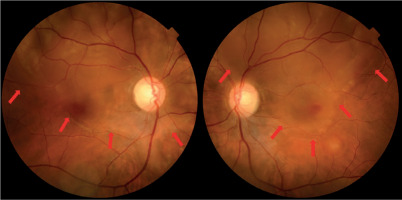
A healthy, 29-year-old female at 39 weeks of her first pregnancy came to the Department of Gynaecology and Obstetrics due to the initiation of labour. The pregnancy was uncomplicated. The patient had no prior ophthalmological history and had never been diagnosed with or treated for any eye-related condition. The patient delivered a healthy baby in natural labour. The child’s birth weight was 3,155 g and it received a 10 Apgar score at 5 minutes of age. There were no neonatal complications. Placental and membrane completeness was confirmed. After completion of the 3rd stage of labour, an increase in the woman’s blood pressure to 160/100 mmHg was observed. Antihypertensive treatment was applied: labetalol (25 mg i.v.), ramipril (5 mg p.o.), and amlodipine (5 mg p.o.). The values of blood pressure were normalized. About 2 hours after delivery, the patient reported headache and visual disturbances in the form of blurry vision. Low-intensity peripheral oedema was observed. The urine analysis revealed proteinuria (450 mg/24 h). Laboratory tests revealed anaemia (hemoglobin level 8.4 g/dl), reduced platelet count (65,000/µl) and increased level of hepatic enzymes (aspartate aminotransferase 48 U/l, alanine aminotransferase 55 U/l). Therefore, the development of the HELLP syndrome secondary to preeclampsia was suspected. Visual problems were becoming more severe and a new symptom of distorted vision appeared, perceived as a “floating image”. Ten hours after delivery the patient underwent an ophthalmological examination. Uncorrected visual acuity (UCVA) was 0.5 for the right eye (RE) and 0.5 for the left eye (LE) at distance, measured using the Snellen chart. Uncor rected visual acuity at near distance was 0.75 for both the RE and LE. Indirect ophthalmoscopy revealed a presence of serous retinal detachment in the upper hemisphere of both eyes with the macula involvement, as well as areas of serous retinal detachment in the peripheral retina (Figure 1). No pathological lesions were found in the optic disc and vessels. The optical coherence tomography (OCT) revealed bilateral neurosensory retinal detachment and a presence of intraretinal oedema. The applied treatment included systemic steroid therapy (prednisone 40 mg p.o. daily), magnesium sulfate (MgSO4 4 g i.m.), and antihypertensive treatment was maintained. The patient remained on bed rest. Over the following days, blood pressure was stabilized and laboratory parameters returned to normal. Visual acuity improved progressively, and the blurring of vision subsided. Follow-up ophthalmological examinations revealed a steady decrease in subretinal fluid and re-attachment of the retina.
Figure 1
Fundus photographs showing bilateral serous retinal detachment taken 1 day after onset. The red arrows indicate the inferior border of the detachment, which appears as a well-demarcated area of retinal elevation due to subretinal fluid accumulation
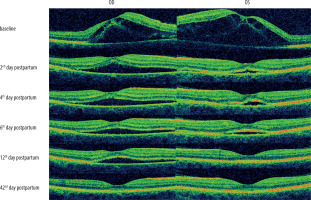
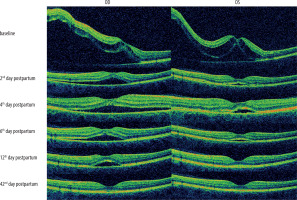
After 7 days of hospitalization, the patient was discharged home with UCVA of 0.7 in the RE and 0.8 in the LE, based on the Snellen chart. Continuation of antihypertensive treatment and steroid therapy was recommended. After 5 weeks, complete regression of subretinal exudate was observed. Best-corrected visual acuity (BCVA) returned to 1.0 in both the RE and the LE, indicating full restoration of visual function. The optical coherence tomography examination showed no structural changes in the foveal region of either eye (Figures 2 and 3).
DISCUSSION
During pregnancy, a female body is subject to a number of physiological changes, both hormonal and metabolic, which affect the course of ophthalmological comorbidities or trigger certain conditions regarding eyesight. The most important ones include characteristic fluctuations in the blood pressure depending on the period of pregnancy, an increase in insulin resistance, which results in poorer glycaemic control, increased blood volume in the vascular bed, increased serum cortisol, and a relative state of hypercoagulability which facilitates the formation of thrombus. Visual disturbances in the course of preeclampsia and eclampsia are common. They affect 25% of patients with preeclampsia and about 50% of patients with eclampsia [4]. The most frequently reported symptom is blurred vision. The others include photopsia, scotomas in the visual field, diplopia, colour vision impairment, sudden difficulty in focusing the eyesight at one point, and in extreme cases development of cortical blindness [4]. In the described case, the patient initially reported blurred vision, which was followed by distorted vision described as a “floating image” – both symptoms are consistent with those commonly reported in literature.
Sometimes, the ocular manifestation is the first symptom of preeclampsia [4]. In our case, the visual symptoms appeared after delivery, about two hours postpartum, when the patient also developed headache and peripheral oedema. This coincided with a diagnosis of proteinuria and laboratory abnormalities consistent with HELLP syndrome. Literature indicates that HELLP can develop during pregnancy or in the postpartum period. In this case, the development occurred after delivery, supporting the notion that postpartum manifestation is clinically relevant and should not be overlooked.
The most common ocular sign observed on ophthalmos-copy is a generalized narrowing of the retinal arterial vessels [4]. Other changes include exudates, small haemorrhages, soft exudates, hard exudates, focal or in the disc region retinal oedema, SRD, acute ischaemic optic neuropathy, and papilledema [2, 4]. In our patient, indirect ophthalmoscopy revealed bilateral serous retinal detachment with macular involvement, along with peripheral retinal detachment, but no abnormalities in the optic disc or vessels were observed. Thus, this case supports literature indicating that SRD may be present as the only abnormality in the posterior segment of the eye, without other features typical of hypertensive retinopathy.
Serous retinal detachment is a rare complication of severe preeclampsia (1–2% of cases) and eclampsia (10% of cases) [5, 6]. According to the American College of Obstetricians and Gynecologists, the presence of SRD is considered to be one of the predictors of severe preeclampsia. Serous retinal detachment occurs seven times more often in patients whose preeclampsia or eclampsia is complicated by the HELLP syndrome compared with preeclampsia without additional complications [2, 6]. In this patient, HELLP syndrome was suspected due to anaemia, thrombocytopenia and elevated liver enzymes, and visual disturbances were among the first clinical manifestations, which is consistent with SRD being a feature of severe disease.
Serous retinal detachment secondary to preeclampsia was first described in 1855 by von Graefe [7], whereas the first reports of SRD secondary to the HELLP syndrome drawn by Burke et al. come from 1989 [5, 6]. Serous retinal detachment is more commonly bilateral, though sometimes unilateral [6, 7]. In our case, SRD was bilateral, with both the macula and peripheral retina involved, aligning with typical presentation. It occurs during pregnancy or in the postpartum period [5] – again, our case demonstrates postpartum onset.
Serous retinal detachment involves the detachment of the sensory retina from the retinal pigment epithelium (RPE) by means of fluid appearing between these two layers. The residual effect of choroidal changes in the course of preeclampsia shown on ophthalmoscopy involves white and yellow spotty RPE deficits and Elschnig spots, which signify past choroidal infarction. These changes may, later in life, mimic macular dystrophy or tapetoid degeneration [5]. In this case, no Elschnig spots or RPE abnormalities were noted during fundoscopic examination or OCT, indicating no signs of chronic choroidal ischaemia. In extreme cases, choroidal ischaemia may lead to the development of necrotic changes in RPE, and in consequence visual field deficits, reduced visual acuity or even permanent blindness [4, 5]. There are contradictory reports in the literature regarding the prognosis for the mother and child in the event of serous retinal detachment secondary to preeclampsia and HELLP syndrome. While some authors suggest that SRD has no prognostic significance for maternal or fetal health, others associate its presence with a poorer prognosis for both [7].
Serous retinal detachment pathogenesis in the course of HDP has not been completely explained. Some authors suggest that the occurrence of SRD results from damage to choroidal vessels due to high blood pressure values [6]. In the case described, blood pressure rose to 160/100 mmHg after delivery. Combined with systemic endothelial dysfunction in HELLP, this may have contributed to choroidal ischemia and increased vascular permeability.
When hypertensive diseases occur during pregnancy, secondary to abnormal placental implantation, there is a release of endogenous factors with a vasospastic effect, which leads to vasoconstriction, damage to vascular endothelial cells by oxidative stress and in consequence, to excessive wall permeability and ischaemia of peripheral tissues [8]. This causes fluid retention in the extracellular space, and leads to cytotoxic and vasogenic oedema, and finally to multiple organ failure secondary to preeclampsia. At the posterior pole of the eye, the vessels become more permeable and the external blood-retinal barrier is disrupted. In the early HDP stages, disorders occur only within the choroidal circulation, excluding retinal vessels. The serous fluid leaking from choriocapillaris accumulates beneath the neuroretina and leads to its detachment [2, 6].
Moreover, in HELLP syndrome, haemolysis causes micro-emboli in choroidal vessels, which further increases ischaemia and the formation of exudates [2]. Moreover, thromboplastin released from the placental system to the mother’s circulation activates the extrinsic coagulation system, causing disseminated intravascular coagulation [2, 5, 8]. Ischaemia causes damage to RPE cells, which lose their ability to transport ions and to reabsorption of fluid from the subretinal space. Additionally, oedema secondary to coexisting hypalbuminaemia facilitated the development of SRD. Thus, it may be claimed that SRD pathogenesis is multifactorial [2, 5]. In our case, serum albumin was low (hypoalbuminaemia), and this, together with increased capillary permeability, likely facilitated fluid accumulation in the subretinal space. Thus, this case further supports the multifactorial pathogenesis of SRD, including vascular damage, hypoalbuminaemia, and endothelial dys-function.
Management of SRD involves prompt treatment of the underlying cause, most commonly preeclampsia and, when present, the HELLP syndrome. The adopted standard procedure included antihypertensive treatment, the use of magnesium sulfate as seizure prophylaxis, and immediate termination of pregnancy, regardless of gestational age (in most cases by way of caesarean section) [9]. In our patient, the adopted strategy included antihypertensive therapy, magnesium sulfate and systemic corticosteroids, and termination of pregnancy had already occurred, which allowed for a focused conservative treatment.
Although systemic steroid therapy is sometimes mentioned in the literature, its effectiveness remains uncertain [9]. In this case, prednisone (Encorton) was used, and progressive improvement in visual acuity and resolution of SRD was observed over time. This suggests potential benefit, although causality cannot be definitively established.
The prognosis regarding visual acuity in this group of patients is generally good. Changes at the posterior pole of the eye regress spontaneously in most cases. It has been reported that complete reabsorption of subretinal fluid and restoration of visual acuity typically occur within 1 to 12 weeks [10]. In the presented case, full regression of SRD and return to baseline visual acuity occurred within 5 weeks, which is consistent with literature data. Best-corrected visual acuity of 1.0 was achieved in both eyes, and no structural abnormalities were seen on follow-up OCT.
CONCLUSIONS
Conditions involving increased blood pressure during pregnancy often result in abnormalities at the posterior pole of the eye. Most of them spontaneously and completely regress when the patient’s general condition is stabilized. Vision disorders in females of childbearing potential, and especially in females with confirmed pregnancy require immediate control of blood pressure and urgent obstetric control. It must be remembered that vision disorders may be the first symptom of developing preeclampsia, which is a serious threat to the life and health of the woman and her child.

 POLSKI
POLSKI