INTRODUCTION
The eyelids are a relatively common site for malignant tumors; however, these lesions are often ignored by patients until they reach a significant size. Malignant eyelid tumors can mimic benign lesions, becoming a diagnostic challenge even for highly experienced oculoplastic surgeons [1, 2]. Eyelid malignancies rarely carry a risk of systemic metastasis and even less frequently serve as a direct cause of patient death. However, when diagnosed and treated late, they require invasive surgical techniques, potentially leading to unfavorable cosmetic outcomes as well as the risk of ocular complications (e.g., exposure keratopathy due to lagophthalmos or ectropion).
The aim of this study was a retrospective analysis of eyelid tumor cases operated on at the Ophthalmology Department, Provincial Hospital in Poznan, Poland.
MATERIAL AND METHODS
The study included 91 patients aged 48 to 90 years (mean 71.45 ±10.47), 61 women aged 48 to 90 (mean 72.33 ±10.86), and 30 men aged 50 to 88 (mean 69.67 ±9.57), who were hospitalized between September 2022 and February 2024 and had lesions suspected of malignancy. All patients provided voluntary and informed consent for the surgery. The research protocol adhered to the principles of the Declaration of Helsinki (1975), as amended in 2000. In all cases, excised lesions were sent for histopathological assessment. In particularly doubtful cases or in patients with surgically difficult-to-define margins, intraoperative histopathological examination of the lesion and its margins was performed.
RESULTS
Surgical resection of eyelid lesions was performed in 83 patients (including 12 cases in which the procedure also involved intraoperative histopathological examination). Due to the presence of orbital tissue infiltration in 2 patients, Vismodegib was used as an adjuvant treatment option. In 8 patients, due to the extensive growth of the lesions observed either during preoperative evaluation and the inability to achieve complete tumour resection, only biopsy samples were collected for histopathological analysis. In 7 biopsy cases, the presence of basal cell carcinoma was confirmed, and the patients were referred for Vismodegib therapy evaluation. In one case, the biopsy showed no evidence of malignancy.
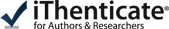
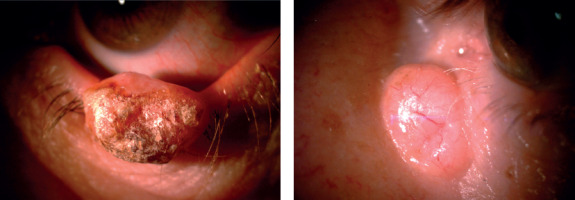
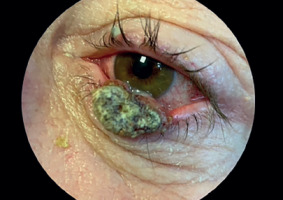
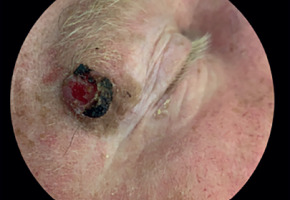
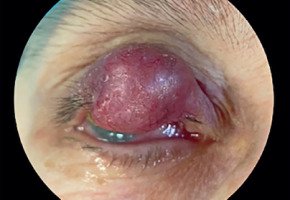
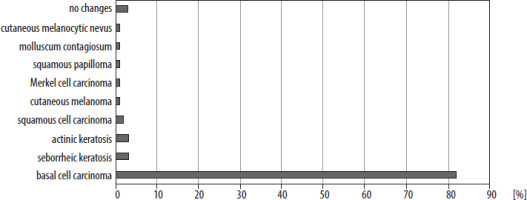
Histopathological examination confirmed the presence of basal cell carcinoma in 75 patients (82.4%; Figure 1A, B). The remaining diagnoses included seborrheic keratosis (3 patients, 3.3%; Figure 2), actinic keratosis (3 patients, 3.3%), squamous cell carcinoma (SCC; 2 patients, 2.2%; Figure 3), cutaneous melanoma (1 patient, 1.1%; Figure 4), Merkel cell carcinoma (1 patient, 1.1%; Figure 5), squamous papilloma (1 patient, 1.1%), molluscum contagiosum (1 patient, 1.1%), and cutaneous melanocytic nevus (1 patient, 1.1%). The histopathological examination did not reveal pathological changes in 3 patients (3.3%) in the study group. The above data are listed in Figure 6.
Among the BCC lesions, which were the most common neoplastic lesions in the study group, 76% were located on the lower eyelid, 16% in the medial canthus, and 8% on the upper eyelid. The most common histopathological subtype of BCC in the analyzed group was the nodular subtype (58.67%). The remaining histopathological subtypes included the infiltrative (13.33%), micronodular (4.00%), metatypical (1.33%), nodular-infiltrative (1.33%), and superficial (1.33%) BCC. In 15 cases, the histopathology report did not include information regarding the subtype of basal cell carcinoma.
The decision to perform intraoperative examination was made if, during preoperative evaluation, the surgeon anticipated a more extensive reconstruction (e.g., involving the periosteum or flaps), when dermatoscopy failed to define lesion margins, and in cases of cancer recurrence. Intraoperative examination was not performed in cases involving well-demarcated lesions confined to the anterior lamella of the eyelid. Of the 12 intraoperative examinations performed, clear margins were found in 6 cases. In 3 cases, although the lesion was completely excised, the surgeon chose to widen the margins. In the remaining 3 patients, due to the presence of cancer cells at the incision line, it was necessary to widen the margins, which was also performed during the procedure, before the reconstruction.
Data concerning the TNM classification of basal cell carcinomas from the final histopathological examination were also analyzed. In 58 cases, the tumors measured less than 2 cm, corresponding to pT1 in the TNM classification. In the remaining cases, the histopathology report did not provide TNM classification data, but only noted the absence of vascular or neural invasion. In 73 cases, the lesion was excised entirely, resulting in negative surgical margins. In contrast, in 2 cases, histopathological examination revealed the presence of cancer cells at the incision line (R1 according to the classification of resection margins, meaning the tumor was macroscopically removed within healthy tissue, but microscopic infiltration remained at the surgical margin) after reconstruction had already been performed. In both cases, intraoperative examination was not undertaken. Reoperation was recommended; however, neither patient returned for the procedure.
Among the cases of squamous cell carcinoma, one patient was diagnosed with the invasive keratinizing G1 subtype, and the other with the invasive keratinizing G2 subtype.
Histopathological examination of a patient with confirmed cutaneous melanoma revealed a tumor invasion depth of 5.5 mm, with involvement of the subcutaneous tissue (pT4b according to the TNM classification). It should also be emphasized that the patient had previously undergone surgical treatment for conjunctival squamous cell carcinoma, which may suggest a significant genetic predisposition to developing malignant lesions.
Merkel cell carcinoma was successfully excised with a 6 mm margin, confirmed by histopathological analysis showing clear margins. The patient was recommended adjuvant radiotherapy; however, this was not administered due to their poor general health. Despite the absence of adjuvant therapy, the patient has remained recurrence-free and metastasis-free for 20 months, underscoring the effectiveness of wide local excision for this aggressive malignancy, even without supplemental treatments.
DISCUSSION
Basal cell carcinoma (BCC) is the most common malignant tumor of the eyelids, accounting for 90% of all malignancies in this region [3]. Solar radiation (ultraviolet light, particularly UVB) is the primary risk factor for the development of BCC. Consequently, these lesions most frequently occur in sun-exposed areas. The lower eyelid and the medial canthus are most commonly affected, with particular prevalence among individuals with lighter skin tones. In the presented study group, BCC lesions also predominantly involved the lower eyelid and medial canthus. Additional risk factors in clude radiation exposure (e.g., from radiotherapy), immunosuppression (including that associated with organ transplantation), pre-existing scars, as well as genetic syndromes such as xeroderma pigmentosum and Gorlin-Goltz syndrome [3].
Several subtypes of BCC can be distinguished, varying in terms of progression and prognosis. The nodular, superficial, micronodular, and infundibulocystic subtypes are associated with a lower likelihood of local recurrence and reduced metastatic potential. In contrast, more aggressive BCC variants include infiltrative, metatypical (basosquamous), and morpheaform subtypes [4, 5]. In the eyelid and periorbital region, the most common forms are the nodular and morpheaform subtypes. The nodular form, which is the most common subtype of BCC (and also the most frequent form in the study group presented in this publication), is a slow-growing and only slightly elevated lesion, appearing as a pearly nodule with dilated surface blood vessels or with ulceration and rolled borders. In contrast, the morpheaform BCC subtype, while less common, frequently demonstrates deeper tissue infiltration (particularly in the medial canthal region where the risk of orbital involvement is greater) and shows higher recurrence rates following primary excision [3]. Moreover, in the diagnosis of morpheaform basal cell carcinoma, the examiner may have difficulty assessing the lesion’s borders, making palpation an extremely important aspect of the examination.
If basal cell carcinoma is suspected based on clinical assessment – including typical macroscopic features, lesion location, and relevant risk factors – the diagnosis must be confirmed through histopathological examination of tissue obtained via biopsy or complete surgical excision.
The 5-year cure rate for BCC is approximately 98%. Factors associated with poorer prognosis include lesions larger than 3 cm, long-term tumor occurrence, deep infiltration, and inadequate treatment [3]. Treatment of periocular basal cell carcinoma involves complete surgical excision of the lesion with an appropriate margin, which can be achieved using either the frozen section technique or Mohs micrographic surgery. Pharmacological methods may also be employed as an alternative to surgical treatment. 5% imiquimod cream is approved for use in the treatment of superficial basal cell carcinoma in adults. The likely mechanism of action of imiquimod involves modification of the immune response and induction of apoptosis in BCC cells. However, studies have demonstrated that treatment of BCC with 5% imiquimod cream is less effective than surgical excision [6]. For locally advanced tumors not amenable to surgery or radiation therapy, as well as in cases of metastatic BCC (which are very rare), vismodegib may be used as a therapeutic option. Vismodegib is an inhibitor of the Hedgehog signaling pathway, which is activated in the majority of basal cell carcinomas but remains inactive in most healthy tissues. This drug has also been used to treat BCC in the periocular and orbital regions, demonstrating effectiveness in nearly half of the studied cases. However, further research is needed to assess, among other aspects, its efficacy in larger patient populations and the potential risk of developing new squamous cell carcinoma lesions in other locations following the completion of therapy [7]. Treatment with vismodegib was initiated in 7 patients from the presented study group. All patients undergoing this therapy showed a positive response to treatment and remain under follow-up.
Seborrheic keratosis is one of the most common benign skin tumors, typically occurring in middle-aged and older individuals. Lesions most frequently appear on the eyelids, forehead, or trunk. Clinically, they present as papules with a characteristic “stuck-on” appearance, a velvety or verrucous surface, and color ranging from beige to brown or black. Their size typically ranges from 3 to 20 mm in diameter [8]. Risk factors for the development of seborrheic keratosis include older age, genetic predisposition, ultraviolet radiation, infection with human papillomavirus (HPV) subtype 16, as well as abnormal lipid or glucose metabolism [9]. The prognosis for seborrheic keratosis is generally very favorable. However, the sudden appearance of multiple lesions – known as the Leser- Trélat sign – is considered a paraneoplastic phenomenon and should prompt thorough diagnostic evaluation for underlying malignant gastrointestinal tumors [10].
Actinic keratosis clinically presents as an erythematous, scaly patch or papule, ranging in size from a few millimeters to 1 cm, usually located on sun-exposed areas of the skin (particularly the face, scalp, forearms, ears, and the backs of the hands) in middle-aged and elderly individuals [11, 12]. Actinic keratosis can progress to squamous cell carcinoma [11].
Squamous cell carcinoma (SCC) is the second most common malignant tumor of the eyelids, after basal cell carcinoma [13]. Risk factors for the development of SCC include older age, exposure to sunlight, petroleum derivatives, tobacco smoke and arsenic, infection with HPV and HIV, as well as actinic keratosis, intraepithelial squamous neoplasia (Bowen’s disease), albinism, and immunosuppression [14]. In cases of squamous cell carcinoma, the lower eyelid is most often affected due to greater sun exposure; however, SCC involves the upper eyelid far more frequently than BCC. Unlike basal cell carcinoma, squamous cell carcinoma is associated with a higher risk of metastasis, particularly to the regional lymph nodes [13].
Merkel cell carcinoma is an extremely rare neuroendocrine malignant skin tumor with a very poor prognosis. This tumor most frequently involves the upper eyelid, typically presenting as a painless, violaceous or reddish-purple nodule with visible telangiectasias. It demonstrates rapid growth (usually within a 6-month period) and a tendency for early metastasis to regional lymph nodes. Risk factors include older age (typically over 50 years), female sex, Caucasian ethnicity, exposure to sunlight, as well as chronic use of TNF-α inhibitors such as adalimumab or golimumab. For surgical excision, wide resection margins (2.5-3 cm) are required, along with biopsy of regional lymph nodes. The available literature includes reports of favorable responses to adjuvant chemotherapy. However, the role of adjuvant radiotherapy remains controversial, as current evidence does not demonstrate a reduction in mortality among patients treated with this modality [15]. Recent studies involving avelumab, a programmed death-ligand 1 (PD-L1) inhibitor, have led to its approval for the treatment of advanced Merkel cell carcinoma [16].
Eyelid skin melanoma is a malignant skin lesion that arises either from the de novo proliferation of cutaneous melanocytes or through the malignant transformation of a preexisting nevus [17]. It should be noted that primary cutaneous melanomas of the eyelids are very rare, accounting for about 1% of all cutaneous melanomas as well as a similarly low percentage of eyelid tumors. In the presented group, melanoma was diagnosed in only one patient. Melanomas of the head and neck typically occur about 20 years later than those in other locations, most often between the ages of 50 and 70. Melanoma of the eyelid skin is more commonly found on the lower eyelid. Risk factors include exposure to ultraviolet light (particularly UVB radiation), fair skin, dysplastic or congenital nevi, positive family history, and advanced age [18]. The primary treatment for early-stage melanoma of the eyelid skin is surgical resection with a wide safety margin. The 10- year survival rate depends on the stage of the disease, ranging from 93% in stage IA (thickness < 0.8 mm, no ulceration) to 10–15% in stage IV (depending on the location of metastases and LDH level) [19].
Melanocytic (pigmented) nevi of the eyelid skin may be either congenital or acquired. Congenital nevi are rare, occurring in only about 1% of newborns. They vary in size, with larger lesions showing an increased tendency toward malignant transformation. Acquired melanocytic nevi appear during childhood and may increase in size as the patient grows. Histologically, nevi are classified into three main types based on the location of melanocyte proliferation: junctional, intradermal, and compound nevi [20]. Because pigmented lesions represent a diverse and heterogeneous group, they often necessitate comprehensive diagnostic evaluation, including histopathological examination, to accurately assess their potential for malignant transformation, as dermatoscopic assessment alone may be insufficient [21].
Squamous cell papilloma represents one of the most common forms of benign conjunctival tumors. The pedunculated form of papilloma, which occurs more frequently in children and young adults, is associated with infection by HPV subtypes 6 and 11. Clinically, it presents as a pinkish-red lesion with a characteristic exophytic growth pattern and only rarely undergoes malignant transformation. In contrast, sessile papillomas are associated with HPV subtypes 16 and 18, show a higher tendency to occur in adults (particularly in the bulbar conjunctiva near the limbus) and are linked to an increased risk of malignant transformation [22].
Molluscum contagiosum virus, belonging to the Poxviridae family, infects skin and mucosal cells, leading to the formation of characteristic umbilicated lesions that may appear, among other locations, on the eyelids. Less commonly, these lesions may occur in the conjunctiva, leading to the development of chronic follicular conjunctivitis as a result of a hypersensitivity reaction [23]. Molluscum contagiosum infection, particularly in immunocompetent individuals, is usually self-limiting. However, in cases of chronic inflammation, removal may be necessary – for example, by curettage [24].
It should be emphasized that all patients in the study group underwent histopathological examination. Based on the findings, appropriate recommendations for further management were issued. Histopathological examination was performed in all cases, including those in which the macroscopic appearance of the lesion did not suggest malignancy.
CONCLUSIONS
Basal cell carcinomas constitute the most common type of malignant tumors of the eyelids. Macroscopic assessment is a very important aspect at the stage of evaluation for surgery, including surgical planning; however, only a thorough histopathological examination allows for establishing the final diagnosis.

 POLSKI
POLSKI