INTRODUCTION
A dermoid cyst (DC) is a benign lesion originating from mature epithelial cells. It arises as a result of abnormal division of embryonic cell layers during embryogenesis. Dermoid cyst is an example of a congenital, non-neoplastic tumor composed of histologically normal and fully mature cells that grow in an abnormal location [1]. It is the most common form of mature teratoma. A DC can develop anywhere in the body; however, it most frequently occurs in the head and neck region (84%) [2].
Dermoid cyst is estimated to account for approximately 3–9% of all orbital tumors and represents the most common benign tumor in this region in the pediatric population (47%) [1, 3, 4]. Around 60-70% of cases are diagnosed before the age of five [2]. The clinical presentation of orbital DC encompasses a wide range of pathological symptoms, depending on its location and size, and associated anomalies. The lesions typically remain asymptomatic for many years and are often detected incidentally during imaging studies performed for other reasons. In this case, the patient underwent an ultrasound examination because visualizing the fundus proved challenging during the diagnostic evaluation for uveitis, which was the primary reason for the patient’s visit to the emergency department.
This study aims to present an unusual case of coexistence between two diseases in a single patient. During the diagnostic evaluation for uveitis, an additional ocular pathology – a DCt of the orbit – was discovered, which had not previously caused any concerning symptoms. To date, no cases of coexistence of these two conditions have been described in the available literature.
CASE REPORT
A 4-year-old patient presented to the ophthalmology emergency department of the University Clinical Hospital in Poznan due to redness in the right eye, which had appeared approximately one week earlier. Based on the medical history and documentation, it was determined that the girl had no chronic illnesses, was developing normally, and had an unremarkable perinatal history. Upon admission, she reported worsening symptoms and the onset of pain in the right eye since the previous day.
Examination revealed reduced visual acuity in the right eye (VOD) at 0.1 and intraocular pressure in both eyes measuring 7 mmHg. A physical examination of the right eye (OD) showed mixed ocular injection (Figure 1). Iris vascular dilation accompanied by posterior synechiae were observed. The cornea was hazy, and small punctate fluorescein-staining areas were observed in the lower hemisphere of its epithelium (likely resulting from the patient rubbing her painful eye). The lens was clear. Inflammatory cells were detected in the anterior chamber. The optical coherence tomography (OCT) scan of the macula was within normal limits. Due to limited visibility of the fundus, an ultrasound of the right eye was performed, revealing an oval hypoechoic mass in the orbit, measuring 17.95 mm × 11.35 mm. The lesion was located in the temporal region (Figure 2). Left eye (OS) examination revealed normal visual acuity, VOS 1.0. The anterior segment and fundus of the OS were within normal limits. For symptomatic management of anterior uveitis in the OD, topical dexamethasone and 1% tropicamide were administered, resulting in partial improvement. Due to significant anisometropia (refraction after 1% cyclopentolate-induced cycloplegia was +6.0 Dsph in the OD and +3.0 Dsph in the OS), the patient was prescribed spectacle correction (OD: +5.0 Dsph; OS: +2.0 Dsph). Ocular biometry revealed axial length discrepancy between OD (19.81 mm) and OS (21.18 mm).
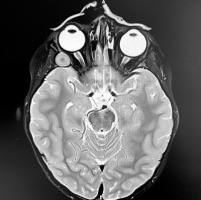
For further evaluation, the patient was referred to the Department of Pediatric Hematology and Oncology at Karol Jonscher Clinical Hospital in Poznan with a diagnosis of iritis and a suspected orbital tumor . A contrast-enhanced magnetic resonance imaging (MRI) scan of the craniofacial region was performed, revealing a well-circumscribed, slightly heterogeneous tumor mass measuring 12 × 11 × 15 mm within the right orbital boundaries, in the area of the greater wing of the sphenoid bone. The lesion demonstrated no post-contrast enhancement and showed no diffusion restriction on DWI/ADC sequences (Figure 3). Orbital computed tomography (CT) revealed bone thinning likely caused by the tumor mass, along with segmental disruption of the orbital walls adjacent to the lesion (Figure 4). The radiological findings raised suspicion of malignancy, leading to a planned biopsy. However, intraoperatively, the tumor’s well-defined margins prompted a decision to proceed with complete tumor resection with the capsule. The subsequent histopathology examination confirmed the diagnosis of DC. Symptomatic treatment for right eye uveitis was continued.
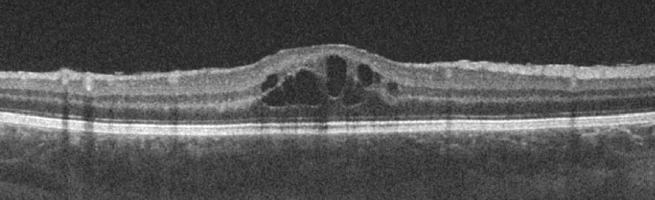
Approximately three weeks after tumor resection, OCT revealed macular edema in the right eye (Figure 5). A steroid (methylprednisolone acetate, Depo-Medrol) was administered via injection under Tenon’s capsule. Two months later, the patient developed left eye uveitis, evidenced by inflammatory cells in the anterior chamber of the left eye.
The girl was referred to the Department of Pediatric Endocrinology and Rheumatology at Poznan University Hospital for further diagnostic evaluation. Laboratory test abnormalities included positive antinuclear antibodies (ANA1 and ANA2) at a titer of 1:320, with a granular fluorescence pattern. An extended ANA panel was negative. Additionally, high levels of anti-thyroid antibodies targeting thyroglobulin (anti-TG) were detected. Tests for HLA-B27 antigen, rheumatoid factor (RF), and angiotensin-converting enzyme (ACE) were negative. Also, there was no evidence of infectious etiology. Ultrasound examination of the thyroid showed signs of inflammation, leading to a diagnosis of Hashimoto’s disease. Substitution therapy with levothyroxine at a dose of 25 μg was initiated. Due to suspected JIA, oral immunosuppressive therapy with methotrexate at a dose of 7.5 mg/day was recommended. The girl remains under the care of ophthalmology, rheumatology, and endocrinology outpatient clinics. The suspicion of JIA has not been confirmed.
Most recent ophthalmic examination demonstrated improved VA in the right eye compared to initial admission testing (current VOD = 1.0). This therapeutic success was achieved through amblyopia treatment following PEDIG guidelines (full refractive correction combined with 2-hour daily patching of the better-seeing eye) and effective local and systemic therapy.
DISCUSSION
The presence of a DC as a congenital defect can be detected at birth. The tumor is characterized by slow growth and often remains asymptomatic for extended periods, which may delay diagnosis. This poses a significant challenge, particularly when the lesion is situated deep within the orbit, as in the reported case. In the described patient, the intraorbital location of the DC caused the relatively large lesion to mold the shape of the globe, resulting in hyperopia and anisometropia, but without affecting eye positioning and external appearance, or producing any other symptoms. Thus, the deep orbital location of the lesion carries a risk of serious complications. Accelerated growth of the DC, typically occurring during adolescence, may lead to a mass effect and compression of the optic nerve or extraocular muscles, potentially resulting in ischemic optic neuropathy, diplopia, exophthalmos, and restricted ocular motility [8, 9]. Cases of spontaneous rupture of orbital DCs have also been described in the literature. The risk of this complication increases with patient age and when DC involves bony structures and leads to localized inflammation [8].
Dermoid cysts most commonly develop superficially, typically in the upper temporal quadrant near the frontozygomatic suture (60–83% of cases) [3]. As a DC enlarges, a subcutaneous mass typically becomes noticeable in the eyebrow or eyelid area, facilitating earlier diagnosis of superficial cysts – often by the age of five – compared to those located deeper [10]. In children and adolescents, superficial DCs often manifest as subtle, well-defined subcutaneous or subconjunctival swellings. Symptoms progress gradually over months. For example, an 18-year-old patient presented with a painless, progressive lower eyelid swelling accompanied by mild exophthalmos persisting for three months. The mass was located in the orbital floor – a rare site for DCs – and showed no signs of compressive symptoms [4].
Imaging studies serve as the cornerstone for diagnosing orbital tumors. While ultrasound is not commonly employed for this purpose, it was utilized in the reported case due to difficulties in evaluating the fundus in our patient. This examination unexpectedly revealed a retrobulbar tumor mass. The MRI and CT are the preferred imaging techniques for evaluating suspected orbital tumors, offering accurate diagnostic insights and valuable guidance for treatment planning [11, 12].
The choice of treatment depends on the tumor’s size and location, and its clinical manifestation. Complete surgical excision remains the preferred approach. Surgery for deeply located orbital DCs can be challenging, often requiring invasive techniques such as microscopic dissection, orbitotomy, or, in rare cases, intracranial exploration [13]. The procedure involves en bloc excision (removal of the cyst as a whole) with an intact capsule to prevent leakage of its contents, which could provoke an acute inflammatory reaction. Complete excision of the DC with clear margins significantly reduces the risk of local recurrence at the surgical site [14, 15].
Uveitis, presenting as eye redness and decreased VA, which was the initial complaint of the patient described in this paper, was likely the first sign of an underlying systemic disease. Potential contributing factors include a positive family history of autoimmune diseases. The patient’s mother has Hashimoto’s disease, which was also diagnosed in the patient during evaluation.
The DC identified in the girl was likely a congenital anomaly that remained asymptomatic, providing no indications for her parents to seek medical evaluation, and was consequently discovered incidentally.
CONCLUSIONS
In this case, the two conditions were distinct pathologies, coincidentally diagnosed simultaneously. A comprehensive understanding of their clinical presentations enabled accurate diagnostic approaches and targeted therapeutic interventions. The case thus highlights that effective collaboration among specialists from different medical fields is crucial.

 POLSKI
POLSKI