INTRODUCTION
Uveal melanoma is the most frequently diagnosed primary intraocular tumor in the adult population with the incidence of 7-8 cases per million white Caucasians [1]. Despite the locally advanced radiotherapy techniques allowing for the eye-sparing treatment in majority of cases, it is estimated that almost 50% of patients will develop distant metastases within 5 years post ocular treatment.
The bilateral occurrence of choroidal melanoma is exceptionally rare [2-4]. The first report comes from United States and was published in 1959 by Wiesinger et al. [5]. The literature on the incidence of bilateral involvement of uveal melanoma is scarce due to the rarity of the condition, the published reports are listed in Table I [5-15]. The second case was published in 1977, also in the United States, by Shammas and Watzke, while at the same time, four other cases were reported in Europe [6].
Table I
A review of the cases of bilateral choroidal melanoma published between 1959-2016 years found in the PubMed database
| Author, reference | Country | Year of the publication | Number of cases | Patient |
|---|---|---|---|---|
| Weisinger et al. [5] | United States | 1959 | 1 | 32-year-old female |
| Shammas et al. [6] | United States | 1977 | 1 | 55-year-old female |
| Migdal et al. [7] | United Kingdom | 1984 | 1 | 51-year-old female |
| Seregard et al. [8] | Sweden | 1988 | 2 | 72-year-old female 86-year-old male |
| Eide [9] | Norway | 1989 | 1 | 73-year-old female |
| Kiratli et al. [10] | Turkey | 2000 | 1 | 76-year-old female |
| Hadden et al. [11] | United Kingdom | 2003 | 4 | 64-year-old female 82-year-old female 75-year-old female 54-year-old female |
| Furuta et al. [12] | United States | 2006 | 3 | 50-year-old male 53-year-old female 92-year-old male |
| Grezda et al. [13] | Albania | 2015 | 1 | 49-year-old female |
| Kowal et al. [14] | Poland | 2015 | 5 | 63-year-old male 49-year-old female 51-year-old female 49-year-old male 39-year-old male |
| Eide et al. [15] | Norway | 2016 | 1 | 72-year-old male |
According to the literature, the estimated frequency of bilateral choroidal melanoma in Europe is one case per 50 million people [7, 16] and the probability of developing this condition in the fellow eye was estimated about 0.2% [16].
The study aims to present two case reports of the patients treated for bilateral choroidal melanoma in our clinic.
MATERIAL AND METHODS
A retrospective analysis was conducted. In each patient, the diagnosis was established based on the ophthalmoscopic image and confirmed with ultrasound examination.
For the follow-up, a comprehensive ophthalmic examination of both eyes was performed in all cases, including best corrected visual acuity (BCVA) assessment, intraocular pressure measurement, slit lamp biomicroscopy and funduscopy. Colour fundus photographies and fundus autofluorescence were captured at each visit to monitor the tumor reaction to radiation treatment. Furthermore, an ultrasonographic examination was carried out to precisely assess the tumor’s dimensions.
At the time of diagnosis, chest X-ray and liver ultrasound were done to check for distant metastases. Then, abdominal ultrasound was repeated every 6 months for moni- toring.
CASE REPORTS
Case report 1
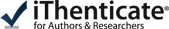
In 2008, a 56-year-old man was referred to our clinic with an intraocular tumor in his right eye (Figure 1 A, C). This was confirmed to be a posterior pole uveal melanoma. Due to the location of the lesion and suspicion of optic nerve involvement, the enucleation of the right eye was performed. Histopathological report following the surgery confirmed the diagnosis of choroidal melanoma with epithelioid cell type predominance. Then, unfortunately, the patient was lost to follow-up for 13 years.
Figure 1
The fundus appearance of the first patient: A) the right eye (May 2008); B) the left eye (May 2021); C, D) the ultrasound of both primary foci of uveal melanoma
He presented in May 2021, due to a deterioration of vision in his fellow eye. At presentation, the BCVA was 0.2 and a collar-stud choroidal melanoma was present in the inferonasal quadrant, penetrating through Bruch’s membrane, measuring 7.74 by 9.48 mm with the thickness of 6.61 mm. The diagnosis of second primary choroidal melanoma of the left eye was made (Figure 1 B, D). The patient underwent Ruthenium-106 (106Ru) brachytherapy of the left eye, followed by transpupillary thermotherapy (TTT). By the time of the last visit in 2023, tumor regressed to the thickness of 4.36 and the BCVA of the left eye improved to 0.4. No distant metastases were detected.
Case report 2
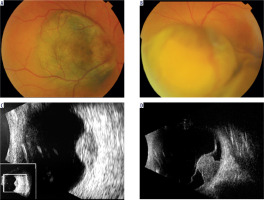
A 54-year-old man was referred in 2017 with the suspicion of intraocular tumor in his right eye. This was diagnosed as a stage T3a choroidal melanoma located superonasally (Figure 2 A, C), measuring 13.69 by 12.96 with the thickness of 10.61 mm. The patient underwent stereotactic radiotherapy (fSRT) with 5 fractions of 10 Gy each, and 2 sessions of transpupillary thermotherapy resulting in tumor regression to the thickness of 3.67 mm. Unfortunately, due to the large size of the irradiated tumor, two years after the radiation treatment, the patient developed a massive toxic tumor syndrome with secondary glaucoma, leading to the loss of light perception.
Figure 2
The fundus appearance of the second patient: A, C) the right eye (May 2017); B) the left eye (January 2023); D) the ultrasound of the second tumor in the left eye
In January 2023, during a routine postoperative follow-up, the choroidal lesion was observed in the upper temporal quadrant of the left eye (mirror-like appearance). This presented ultrasound features of small uveal melanoma, with dimensions of 11.73 × 8.13 mm and the thickness of 2.29 mm (Figure 2 B, D). At that time, the visual acuity of the left eye was 0.8. Based on the clinical image and ultrasonographic examination, the diagnosis of choroidal melanoma T1a in the fellow eye was established and brachytherapy with 106Ru of the left eye was performed. At the last follow-up visit, the vision was 1.0 in that eye and the tumor regression was visible.
DISCUSSION
This is a report of two exceedingly rare cases of bilateral uveal melanoma. The diagnosis in each patient was made after a fundus examination and ophthalmic ultrasound.
The time from the appearance of the primary tumor to the diagnosis of second choroidal melanoma in the fellow eye in our patients was 10 and 6 years, respectively. With the cases published in the literature, the time between the appearance of a tumor in the fellow eye and the occurrence of choroidal melanoma in the first eye ranged from 1 to 5 years [17], 0-6 with an average of 2 years [18]. However, there are some reports of the second tumor appearing even after over 30 years from the first diagnosis [16].
There are likely other factors responsible for the bilaterality of choroidal melanoma than just randomness. Genetic factors may play a role in the development of bilateral choroidal melanomas, and unidentified germinal mutations might be involved in their pathogenesis [4, 18]. The bilateral occurrence of primary tumors suggests a hereditary predisposition to tumorigenesis. Sequencing of highly metastatic choroidal melanomas revealed an associated inactivating mutation in the gene encoding the BRCA1-associated protein 1 (BAP1) [4, 15, 18-21]. This discovery suggests that the mutation in BAP1 gene and subsequent loss of BAP1 protein might be linked to bilateral occurrence of choroidal melanoma. Yu et al. proposed the „rule of twos” concerning the potential genetic basis of bilateral choroidal melanoma, as a guideline for conducting tests for the presence of BAP-1 mutations (which probably predispose to bilateral choroidal melanoma occurrence). The rule is to test patients with two or more BAP1-associated cancers (especially advanced uveal melanoma of the eye, cutaneous melanoma, renal cell carcinoma, or mesothelioma) in one patient, or with two or more suspected primary uveal melanoma foci in one eye (multifocal) or both eyes (bilateral), or patients with two or more family members (first or second degree of consanguinity) with BAP1-associated tumors [4].
It has been observed that ocular melanocytosis increases the risk of choroidal melanoma and occurs more frequently in bilateral choroidal melanomas (25%) than in unilateral cases (1.3%) [5]. Pre-existing ocular melanocytosis has been described in 12-25% of patients with bilateral choroidal melanoma [4], however it was not present in any of our patients. Also some environmental factors that have been proposed to influence the increased risk of bilateral choroidal melanoma include arc welding and immunosuppression [4].
None of our patients developed metastases so far. According to the literature, patients with unilateral choroidal melanoma had similar survival rates as those with bilateral involvement [22].
CONCLUSIONS
In rare cases, choroidal melanoma can occur bilaterally. It is essential to pay attention to the fellow eye of the patient during routine postoperative follow-up. The observation period should be long because there have been reported cases of this tumor appearing in the fellow eye even after 30 years [6].
Some authors suggest the relevance of conducting tests for the presence of germinal BAP-1 mutations in cases of bilateral choroidal melanoma [4].

 POLSKI
POLSKI